Multiple sclerosis
From Wikipedia, the free encyclopedia
| Multiple sclerosis | |
|---|---|
| Classification and external resources | |
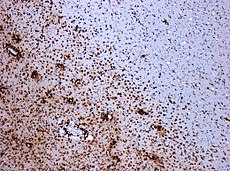 Demyelination by MS. The CD68 colored tissue shows several macrophages in the area of the lesion. Original scale 1:100 | |
| ICD-10 | G35 |
| ICD-9 | 340 |
| OMIM | 126200 |
| DiseasesDB | 8412 |
| MedlinePlus | 000737 |
| eMedicine | neuro/228 oph/179emerg/321 pmr/82radio/461 |
| MeSH | D009103 |
| GeneReviews | |
Multiple sclerosis (MS), also known as "disseminated sclerosis" or "encephalomyelitis disseminata", is an inflammatory disease in which the fattymyelin sheaths around the axons of the brain and spinal cord are damaged, leading to demyelination and scarring as well as a broad spectrum ofsigns and symptoms.[1] Disease onset usually occurs in young adults, and it is more common in women.[1] It has a prevalence that ranges between 2 and 150 per 100,000.[2] MS was first described in 1868 by Jean-Martin Charcot.[3]
MS affects the ability of nerve cells in the brain and spinal cord to communicate with each other effectively. Nerve cells communicate by sending electrical signals called action potentials down long fibers called axons, which are contained within an insulating substance called myelin. In MS, the body's own immune system attacks and damages the myelin. When myelin is lost, the axons can no longer effectively conduct signals.[4] The namemultiple sclerosis refers to scars (sclerae-—better known as plaques or lesions) particularly in the white matter of the brain and spinal cord, which is mainly composed of myelin.[3] Although much is known about the mechanisms involved in the disease process, the cause remains unknown. Theories include genetics or infections. Different environmental risk factors have also been found.[4][5]
Almost any neurological symptom can appear with the disease, and the disease often progresses to physical and cognitive disability.[4] Psychiatric symptoms and difficult thinking may also occur.[6] MS takes several forms, with new symptoms occurring either in discrete attacks (relapsing forms) or accumulating over time (progressive forms).[7] Between attacks, symptoms may go away completely, but permanent neurological deficits often occur, especially as the disease advances.[7]
There is no known cure for multiple sclerosis. Treatments attempt to return function after an attack, prevent new attacks, and prevent disability.[4] MS medications can have adverse effects or be poorly tolerated, and many people pursue alternative treatments, despite the lack of supporting scientific study. The prognosis is difficult to predict; it depends on the subtype of the disease, the individual's disease characteristics, the initial symptoms and the degree of disability the person experiences as time advances.[8] Life expectancy of people with MS is 5 to 10 years lower than that of the unaffected population.[1]
Contents[hide] |
Signs and symptoms
Main article: Multiple sclerosis signs and symptoms
A person with MS can suffer almost any neurological symptom or sign, including changes in sensation such as loss of sensitivity or tingling, pricking or numbness (hypoesthesia and paresthesia), muscle weakness, clonus, muscle spasms, or difficulty in moving; difficulties with coordination and balance (ataxia); problems in speech (dysarthria) or swallowing (dysphagia), visual problems (nystagmus, optic neuritis including phosphenes,[9][10] or diplopia),fatigue, acute or chronic pain, and bladder and bowel difficulties.[1] Cognitive impairment of varying degrees and emotional symptoms of depression orunstable mood are also common.[1] Uhthoff's phenomenon, an exacerbation of extant symptoms due to an exposure to higher than usual ambient temperatures, and Lhermitte's sign, an electrical sensation that runs down the back when bending the neck, are particularly characteristic of MS although not specific.[1] The main clinical measure of disability progression and symptom severity is the Expanded Disability Status Scale or EDSS.[11]
Symptoms of MS usually appear in episodic acute periods of worsening (called relapses, exacerbations, bouts, attacks, or "flare-ups"), in a gradually progressive deterioration of neurologic function, or in a combination of both.[7] Multiple sclerosis relapses are often unpredictable, occurring without warning and without obvious inciting factors with a rate rarely above one and a half per year.[1] Some attacks, however, are preceded by common triggers. Relapses occur more frequently during spring and summer.[12] Viral infections such as the common cold, influenza, or gastroenteritis increase the risk of relapse.[1] Stress may also trigger an attack.[13] Pregnancy affects the susceptibility to relapse, with a lower relapse rate at each trimester of gestation. During the first few months after delivery, however, the risk of relapse is increased.[1] Overall, pregnancy does not seem to influence long-term disability. Many potential triggers have been examined and found not to influence MS relapse rates. There is no evidence that vaccination and breast feeding,[1] physical trauma,[14] or Uhthoff's phenomenon[12] are relapse triggers.
Causes
Most likely MS occurs as a result of some combination of genetic, environmental and infectious factors,[1] and possibly other factors like vascular problems.[15] Epidemiological studies of MS have provided hints on possible causes for the disease. Theories try to combine the known data into plausible explanations, but none has proved definitive.
Genetics
MS is not considered a hereditary disease. However, a number of genetic variations have been shown to increase the risk of developing the disease.[16]
The risk of acquiring MS is higher in relatives of a person with the disease than in the general population, especially in the case of siblings, parents, and children.[4] The disease has an overall familial recurrence rate of 20%.[1] In the case of monozygotic twins, concordance occurs only in about 35% of cases, while it goes down to around 5% in the case of siblings and even lower in half-siblings. This indicates susceptibility is partly polygenicallydriven.[1][4] It seems to be more common in some ethnic groups than others.[17]
Apart from familial studies, specific genes have been linked with MS. Differences in the human leukocyte antigen (HLA) system—a group of genes inchromosome 6 that serves as the major histocompatibility complex (MHC) in humans—increase the probability of suffering MS.[1] That changes in the HLA region are related to the susceptibility of an individual for MS has been known for over thirty years,[18] and additionally this same region has been implicated in the development of other autoinmmune diseases such as diabetes type I and systemic lupus erythematosus.[18] The most consistent finding is the association between multiple sclerosis and alleles of the MHC defined as DR15 and DQ6.[1] Other loci have shown a protective effect, such as HLA-C554 and HLA-DRB1*11.[1] Overall, it has been stimated that HLA changes accounts for between 20 and 60% of the genetic predisposition for MS.[18] Modern genetic methods (Genome-wide association studies, or GWAS) have also permitted to discover at least 12 other genes outside the HLA locus that modestly increase the probability of suffering MS.[18]
Environmental factors
Different environmental factors, both of infectious and non-infectious origin, have been proposed as risk factors for MS. Although some are partly modifiable, only further research—especially clinical trials—will reveal whether their elimination can help prevent MS.[19]
MS is more common in people who live farther from the equator, although many exceptions exist.[1] Decreased sunlight exposure has been linked with a higher risk of MS.[19] Decreased vitamin D production and intake has been the main biological mechanism used to explain the higher risk among those less exposed to sun.[19][20][21]
Severe stress may be a risk factor although evidence is weak.[19] Smoking has also been shown to be an independent risk factor for developing MS.[20]Association with occupational exposures and toxins—mainly solvents—has been evaluated, but no clear conclusions have been reached.[19]Vaccinations were investigated as causal factors for the disease; however, most studies show no association between MS and vaccines.[19] Several other possible risk factors, such as diet[22] and hormone intake, have been investigated; however, evidence on their relation with the disease is "sparse and unpersuasive".[20]
Gout occurs less than would statistically be expected in people with MS, and low levels of uric acid have been found in people with MS as compared to normal individuals. This led to the theory that uric acid protects against MS, although its exact importance remains unknown.[23]
Infections
Many microbes have been proposed as potential infectious triggers of MS, but none have been substantiated.[4] Moving at an early age from one location in the world to another alters a person's subsequent risk of MS.[5] An explanation for this could be that some kind of infection, produced by a widespread microbe rather than a rare pathogen, is the origin of the disease.[5] There are a number of proposed mechanisms, including the hygiene hypothesis and the prevalence hypothesis. The hygiene hypothesis proposes that exposure to several infectious agents early in life is protective against MS, the disease being a response to a later encounter with such agents.[1] The prevalence hypothesis proposes that the disease is due to a pathogen more common in regions of high MS prevalence where in most individuals it causes an asymptomatic persistent infection. Only in a few cases and after many years does it cause demyelination.[5][24] The hygiene hypothesis has received more support than the prevalence hypothesis.[5]
Evidence for viruses as a cause includes the presence of oligoclonal bands in the brain and cerebrospinal fluid of most people with MS, the association of several viruses with human demyelinationencephalomyelitis, and induction of demyelination in animals through viral infection.[25] Human herpes viruses are a candidate group of viruses linked to MS. Individuals who have never been infected by the Epstein-Barr virus have a reduced risk of having the disease, and those infected as young adults have a greater risk than those who had it at a younger age.[1][5] Although some consider that this goes against the hygiene hypothesis, since the noninfected have probably experienced a more hygienic upbringing,[5] others believe that there is no contradiction since it is a first encounter at a later moment with the causative virus that is the trigger for the disease.[1] Other diseases that have also been related with MS are measles, mumps, and rubella.[1]
Pathophysiology
Main article: Pathophysiology of multiple sclerosis
Autoimmunology
MS is believed to be an immune-mediated disorder mediated by a complex interaction of the individual's genetics and as yet unidentified environmental insults.[4] Damage is believed to be caused by the person's own immune system attacking the nervous system. Possible targets of the immune response include myelin basic protein (MBP) and proteolipid protein (PLP). The commonly prescribed MS drug Copaxone was designed to mimic MBP and therefore act as a decoy for autoreactive immune cells. Even so, the role of MBP in MS is controversial; it is buried within the myelin sheath (rather than on the surface), where immune cells would not be able to recognize it.
Recent data suggest a role for myelin lipids in MS.[26] Historically, researchers have assumed the myelin target was a protein, even though the myelin sheath is nearly 80% lipid. Furthermore, lipids are known to be the target of another prominent nervous system autoimmune condition, Guillain-Barre Syndrome.
Whether the autoantigen is a protein or a lipid, autoimmunity may arise when immune cells recognizing a foreign antigen cross-react with self antigens. This process is known as molecular mimicry.[4][27]
Lesions
The name multiple sclerosis refers to the scars (sclerae – better known as plaques or lesions) that form in the nervous system. MS lesions most commonly involve white matter areas close to theventricles of the cerebellum, brain stem, basal ganglia and spinal cord; and the optic nerve. The function of white matter cells is to carry signals between grey matter areas, where the processing is done, and the rest of the body. The peripheral nervous system is rarely involved.[4]
More specifically, MS destroys oligodendrocytes, the cells responsible for creating and maintaining a fatty layer—known as the myelin sheath—which helps the neurons carry electrical signals(action potentials).[4] MS results in a thinning or complete loss of myelin and, as the disease advances, the cutting (transection) of the neuron's axons. When the myelin is lost, a neuron can no longer effectively conduct electrical signals.[4] A repair process, called remyelination, takes place in early phases of the disease, but the oligodendrocytes cannot completely rebuild the cell's myelin sheath.[28] Repeated attacks lead to successively fewer effective remyelinations, until a scar-like plaque is built up around the damaged axons.[28] Different lesion patterns have been described.[29]
Inflammation
Apart from demyelination, the other pathologic hallmark of the disease is inflammation. According to a strictly immunological explanation of MS, the inflammatory process is caused by T cells, a kind of lymphocyte. Lymphocytes are cells that play an important role in the body's defenses.[4] In MS, T cells gain entry into the brain via disruptions in the blood–brain barrier. Evidence from animal models also point to a role of B cells in addition to T cells in development of the disease.[30]
The T cells recognize myelin as foreign and attack it as if it were an invading virus. This triggers inflammatory processes, stimulating other immune cells and soluble factors like cytokines andantibodies. Further leaks form in the blood–brain barrier, which in turn cause a number of other damaging effects such as swelling, activation of macrophages, and more activation of cytokines and other destructive proteins.[4]
Blood–brain barrier breakdown
The blood–brain barrier is a part of the capillary system that prevents the entry of T cells into the central nervous system.[4] However, it may become permeable to these types of cells because of an infection or a virus.[4] When the blood–brain barrier regains its integrity, typically after the infection or virus has cleared, the T cells are trapped inside the brain.[4]
Diagnosis
Multiple sclerosis can be difficult to diagnose since its signs and symptoms may be similar to other medical problems.[1][31] Medical organizations have created diagnostic criteria to ease and standardize the diagnostic process especially in the first stages of the disease.[1] Historically, the Schumacher and Poser criteria were both popular.[32]
Currently, the McDonald criteria focus on a demonstration with clinical, laboratory and radiologic data of the dissemination of MS lesions in time and space for non-invasive MS diagnosis, though some have stated that the only proved diagnosis of MS is autopsy, or occasionally biopsy, where lesions typical of MS can be detected through histopathological techniques.[1][33][34]
Clinical data alone may be sufficient for a diagnosis of MS if an individual has suffered separate episodes of neurologic symptoms characteristic of MS.[33] Since some people seek medical attention after only one attack, other testing may hasten and ease the diagnosis. The most commonly used diagnostic tools are neuroimaging, analysis of cerebrospinal fluid and evoked potentials. Magnetic resonance imaging of the brain and spine shows areas of demyelination (lesions or plaques). Gadolinium can be administered intravenously as a contrast to highlight active plaques and, by elimination, demonstrate the existence of historical lesions not associated with symptoms at the moment of the evaluation.[33][35] Testing of cerebrospinal fluid obtained from alumbar puncture can provide evidence of chronic inflammation of the central nervous system. The cerebrospinal fluid is tested for oligoclonal bands of IgG on electrophoresis, which are inflammation markers found in 75–85% of people with MS.[33][36] The nervous system of a person with MS responds less actively to stimulation of the optic nerve and sensory nerves due to demyelination of such pathways. These brain responses can be examined using visual and sensory evoked potentials.[37]
Clinical courses
Several subtypes, or patterns of progression, have been described. Subtypes use the past course of the disease in an attempt to predictthe future course. They are important not only for prognosis but also for therapeutic decisions. In 1996 the United States National Multiple Sclerosis Society standardized four clinical courses:[7]
- relapsing remitting,
- secondary progressive,
- primary progressive, and
- progressive relapsing.
The relapsing-remitting subtype is characterized by unpredictable relapses followed by periods of months to years of relative quiet (remission) with no new signs of disease activity. Deficits suffered during attacks may either resolve or leave sequelae, the latter being more common as a function of time.[1] This describes the initial course of 80% of individuals with MS.[1] When deficits always resolve between attacks, this is sometimes referred to as benign MS,[38] although people will still accrue some degree of disability in the long term.[1] On the other hand, the term malignant multiple sclerosis is used to describe MS patients who reach significant level of disability in a short period of time.[39] The relapsing-remitting subtype usually begins with a clinically isolated syndrome (CIS). In CIS, a person has an attack suggestive of demyelination, but does not fulfill the criteria for multiple sclerosis.[1][40] However only 30 to 70% of persons experiencing CIS later develop MS.[40]
Secondary progressive MS describes around 65% of those with an initial relapsing-remitting MS, who then begin to have progressive neurologic decline between acute attacks without any definite periods of remission.[1][7] Occasional relapses and minor remissions may appear.[7]The median time between disease onset and conversion from relapsing-remitting to secondary progressive MS is 19 years.[41] The primary progressive subtype describes the approximately 10–15% of individuals who never have remission after their initial MS symptoms.[42] It is characterized by progression of disability from onset, with no, or only occasional and minor, remissions and improvements.[7] The age of onset for the primary progressive subtype is later than for the relapsing-remitting, but similar to mean age of progression between the relapsing-remitting and the secondary progressive. In both cases it is around 40 years of age.[1]
Progressive relapsing MS describes those individuals who, from onset, have a steady neurologic decline but also suffer clear superimposed attacks. This is the least common of all subtypes.[7]
Atypical variants of MS with non-standard behavior have been described; these include Devic's disease, Balo concentric sclerosis, Schilder's diffuse sclerosis and Marburg multiple sclerosis. There is debate on whether they are MS variants or different diseases.[43] Multiple sclerosis also behaves differently in children, taking more time to reach the progressive stage.[1] Nevertheless they still reach it at a lower mean age than adults.[1]
Management
Main article: Treatment of multiple sclerosis
Although there is no known cure for multiple sclerosis, several therapies have proven helpful. The primary aims of therapy are returning function after an attack, preventing new attacks, and preventing disability. As with any medical treatment, medications used in the management of MS have several adverse effects. Alternative treatments are pursued by some people, despite the shortage of supporting, comparable, replicated scientific study.
Acute attacks
During symptomatic attacks, administration of high doses of intravenous corticosteroids, such as methylprednisolone, is the routine therapy for acute relapses,[1] while oral corticosteroids seem to have a similar efficacy and safety profile.[44] Although generally effective in the short term for relieving symptoms, corticosteroid treatments do not appear to have a significant impact on long-term recovery.[45] Consequences of severe attacks which do not respond to corticosteroids might be treated by plasmapheresis.[1]
Disease-modifying treatments
As of April 2013, eight disease-modifying treatments have been approved by regulatory agencies of different countries. The approved drugs are interferon beta-1a, interferon beta-1b, glatiramer acetate, mitoxantrone, natalizumab, fingolimod, teriflunomide and dimethyl fumarate.[1][46][47][48][49]
The interferons and glatiramer acetate are delivered by frequent injections, varying from once-per-day for glatiramer acetate to once-per-week (but intra-muscular) for interferon beta-1a. Natalizumab and mitoxantrone are given by intravenous (IV) infusion at monthly intervals in the case of natalizumab and every three months in the case of mitoxantrone.[50][51][52] In 2010 fingolimod became the first oral drug approved by the FDA,[46] being followed by teriflunomide and dimethyl fumarate.[47][48] Fingolimod and teriflunomide are taken through a daily single dose whereas dimethyl fumarate is administered twice daily.[47][48][53] Most drugs are approved only for the relapsing-remitting course (RRMS). Medications are modestly effective at decreasing the number of attacks in RRMS.[54]
Interferons and glatiramer acetate are roughly equivalent, reducing relapses by approximately 30%.[1] Comparisons to natalizumab show that the most effective is the latter, both in terms of relapse rate reduction and halting disability progression.[55] Mitoxantrone may be the most effective of them all; however, it is generally not considered as a long-term therapy, as its use is limited by severe secondary effects.[1][56] While more studies of the long-term effects of the drugs are needed,[1][56][57] specially for the newest treatments, existing data on the effects of interferons and glatiramer acetate indicate that early-initiated long-term therapy is safe and it is related to better outcomes.[57][58]
The earliest clinical presentation of RRMS is the clinically isolated syndrome (CIS). Treatment with interferons during an initial attack decreases the chance that a person will develop clinical MS.[1][59] Treatment of progressive MS is more difficult than relapsing-remitting MS. Mitoxantrone has shown positive effects in those with secondary progressive and progressive relapsing courses. It is moderately effective in reducing the progression of the disease and the frequency of relapses in short-term follow-up.[60] No treatment has been proven to modify the course of primary progressive MS.[61]Efficacy of most common treatments, interferons and glatiramer acetate, in early-onset MS (before eighteen years of age) has been estimated to be roughly equivalent to adults.[62]
As with many medical treatments, these treatments have several adverse effects. One of the most common is irritation at the injection site for glatiramer acetate and the interferon treatments. Over time, a visible dent at the injection site, due to the local destruction of fat tissue, known as lipoatrophy, may develop. Interferons produce symptoms similar to influenza;[63] some people taking glatiramer experience a post-injection reaction manifested by flushing, chest tightness, heart palpitations, breathlessness, and anxiety, which usually lasts less than thirty minutes.[64] More dangerous but much less common are liver damage from interferons,[65] severe cardiotoxicity, infertility, and acute myeloid leukemia of mitoxantrone,[1][56] and the putative link between natalizumab and some cases of progressive multifocal leukoencephalopathy.[1]
Fingolimod may give rise to hypertension and bradycardia, macular edema, elevated liver enzymes or reduction in lymphocite levels.[66] Teriflunomide is considered a very safe drug. Nevertheless there have been reports of liver failure and PML and it is dangerous for fetal development.[66] Most common secondary effects of dimethyl fumarate are flushing and gastrointestinal problems.[48] While dimethyl fumarate leads to a reduction in white blood cell count there were no reported cases of opportunistic infections during clinical trials.[48]
Associated symptoms
Disease-modifying treatments reduce the progression rate of the disease, but do not stop it. As multiple sclerosis progresses, the symptomatology tends to increase. The disease is associated with a variety of symptoms and functional deficits that result in a range of progressive impairments and disability. Management of these deficits is therefore very important. Both drug therapy and neurorehabilitation have shown to ease the burden of some symptoms, though neither influences disease progression.[1][67] Some symptoms have a good response to medication, such as unstable bladder and spasticity, while management of many others is much more complicated.[1] As for any person with neurologic deficits, amultidisciplinary approach is key to improving quality of life; however, there are particular difficulties in specifying a 'core team' because people with MS may need help from almost any health profession or service at some point.[1] Multidisciplinary rehabilitation programs increase activity and participation of people with MS but do not influence impairment level.[68] Due to the paucity of randomized controlled studies, there is limited evidence of the overall efficacy of individual therapy disciplines,[69][69][70] though there is good evidence that specific approaches, such as exercise,[71][72] psychology therapies, particularly cognitive behavioral approaches[73] and energy conservation instruction[74] are effective.
Alternative treatments
Over 50% of MS patients may use complementary and alternative medicine, although numbers vary greatly depending on the definition of alternative medicine used.[75] The evidence for effectiveness for such treatments in most cases is weak or absent.[75][76] Examples of treatments used by patients with unproven efficacy are dietary supplementation and regimens,[75][77]relaxation techniques such as yoga,[75] herbal medicine (including the use of medical cannabis),[75][78] hyperbaric oxygenation,[79] self-infection with hookworm (known generally as helminthic therapy), reflexology or acupunture.[75][80] Regarding the characteristics of users, they are more frequently women, have had MS for a longer time and tend to be more disabled. Moreover, they also have lower levels of satisfaction with conventional healthcare.[75]
Prognosis
The prognosis (the expected future course of the disease) for a person with multiple sclerosis depends on the subtype of the disease; the individual's sex, age, and initial symptoms; and the degree of disability the person experiences.[8] The disease evolves and advances over decades, 30 being the mean years to death since onset.[1]
Female sex, relapsing-remitting subtype, optic neuritis or sensory symptoms at onset, few attacks in the initial years and especially early age at onset, are associated with a better course.[8][81]
The life expectancy of people with MS is 5 to 10 years lower than that of unaffected people.[1] Almost 40% of people with MS reach the seventh decade of life.[81] Nevertheless, two-thirds of the deaths in people with MS are directly related to the consequences of the disease.[1] Suicide also has a higher prevalence than in the healthy population, while infections and complications are especially hazardous for the more disabled ones.[1]
Although most people lose the ability to walk before death, 90% are still capable of independent walking at 10 years from onset, and 75% at 15 years.[81][82]
Epidemiology
Two main measures are used in epidemiological studies: incidence and prevalence. Incidence is the number of new cases per unit of person–time at risk (usually number of new cases per thousand person–years); while prevalence is the total number of cases of the disease in the population at a given time. Prevalence is known to depend not only on incidence, but also on survival rate and migrations of affected people. MS has a prevalence that ranges between 2 and 150 per 100,000 depending on the country or specific population.[2] Studies on populational and geographical patterns of epidemiological measures have been very common in MS,[24] and have led to the proposal of different etiological (causal) theories.[5][19][20][24]
MS usually appears in adults in their thirties but it can also appear in children.[1] The primary progressive subtype is more common in people in their fifties.[42] As with many autoimmune disorders, the disease is more common in women, and the trend may be increasing.[1][83] The CDC data suggest that MS is three times more common in women than in men in the United States.[84] In children, the sex ratio difference is higher,[1] while in people over fifty, MS affects males and females almost equally.[42]
There is a north-to-south gradient in the northern hemisphere and a south-to-north gradient in the southern hemisphere, with MS being much less common in people living near the equator.[1][83]Climate, sunlight and intake of vitamin D have been investigated as possible causes of the disease that could explain this latitude gradient.[20] However, there are important exceptions to the north–south pattern and changes in prevalence rates over time;[1] in general, this trend might be disappearing.[83] This indicates that other factors such as environment or genetics have to be taken into account to explain the origin of MS.[1] MS is also more common in regions with northern European populations.[1] But even in regions where MS is common, some ethnic groups are at low risk of developing the disease, including the Samis, Turkmen, Amerindians, Canadian Hutterites, Africans, and New Zealand Māori.[85]
Environmental factors during childhood may play an important role in the development of MS later in life. Several studies of migrants show that if migration occurs before the age of 15, the migrant acquires the new region's susceptibility to MS. If migration takes place after age 15, the migrant retains the susceptibility of his home country.[1][19] However, the age–geographical risk for developing multiple sclerosis may span a larger timescale.[1] A relationship between season of birth and MS has also been found which lends support to an association with sunlight and vitamin D. For example fewer people with MS are born in November as compared to May.[86]
History
Medical discovery
The French neurologist Jean-Martin Charcot (1825–1893) was the first person to recognize multiple sclerosis as a distinct disease in 1868.[87]Summarizing previous reports and adding his own clinical and pathological observations, Charcot called the disease sclerose en plaques. The three signs of MS now known as Charcot's triad 1 are nystagmus, intention tremor, and telegraphic speech (scanning speech), though these are not unique to MS. Charcot also observed cognition changes, describing his patients as having a "marked enfeeblement of the memory" and "conceptions that formed slowly".[3]
Before Charcot, Robert Carswell (1793–1857), a British professor of pathology, and Jean Cruveilhier (1791–1873), a French professor of pathologic anatomy, had described and illustrated many of the disease's clinical details, but did not identify it as a separate disease.[87] Specifically, Carswell described the injuries he found as "a remarkable lesion of the spinal cord accompanied with atrophy".[1] Under the microscope, Swiss pathologist Georg Eduard Rindfleisch (1836–1908) noted in 1863 that the inflammation-associated lesions were distributed around blood vessels.[88][89]
After Charcot's description, Eugène Devic (1858–1930), Jozsef Balo (1895–1979), Paul Ferdinand Schilder (1886–1940), and Otto Marburg (1874–1948) described special cases of the disease. During all the 20th century there was an important development on the theories about the cause and pathogenesis of MS while efficacious treatments began to appear in 1990.[1]
Historical cases
There are several historical accounts of people who lived before or shortly after the disease was described by Charcot and probably had MS.
A young woman called Halldora who lived in Iceland around 1200 suddenly lost her vision and mobility but, after praying to the saints, recovered them seven days after. Saint Lidwina of Schiedam (1380–1433), a Dutch nun, may be one of the first clearly identifiable MS patients. From the age of 16 until her death at 53, she suffered intermittent pain, weakness of the legs, and vision loss—symptoms typical of MS.[90] Both cases have led to the proposal of a 'Viking gene' hypothesis for the dissemination of the disease.[91]
Augustus Frederick d'Este (1794–1848), son of Prince Augustus Frederick, Duke of Sussex and Lady Augusta Murray and the grandson of George III of the United Kingdom, almost certainly suffered from MS. D'Este left a detailed diary describing his 22 years living with the disease. His diary began in 1822 and ended in 1846, although it remained unknown until 1948. His symptoms began at age 28 with a sudden transient visual loss (amaurosis fugax) after the funeral of a friend. During the course of his disease, he developed weakness of the legs, clumsiness of the hands, numbness, dizziness, bladder disturbances, and erectile dysfunction. In 1844, he began to use a wheelchair. Despite his illness, he kept an optimistic view of life.[92][93]
Another early account of MS was kept by the British diarist W. N. P. Barbellion, nom-de-plume of Bruce Frederick Cummings (1889–1919), who maintained a detailed log of his diagnosis and struggle with MS.[93] His diary was published in 1919 as The Journal of a Disappointed Man.[94]
Research
Main article: Therapies under investigation for multiple sclerosis
There have been important advances in the research of multiple sclerosis in the last decade that have led to a deeper comprenhension of the disease mechanisms and also to more effective treatments.[95] Nevertheless, MS continues to be an active field of research.[95]
Diagnosis and disease biomarkers
Regarding diagnosis it is not expected that diagnostic criteria may change in the near future. On the other hand, while the search for biomarkers of the disease that may aid diagnosis, prediction of disease evolution,or evaluation of disease evolution, is intense there are not any expected breakthroughs in the short term.[95]
The variable clinical presentation of MS and the lack of diagnostic laboratory tests lead to delays in diagnosis and the impossibility of predicting diagnosis. New diagnostic methods that are being investigated include work with anti-myelin antibodies, and studies with serum and cerebrospinal fluidbut none of them has yielded reliable positive results.[97]
Currently there are no clinically established laboratory investigations available that can predict prognosis. However, several promising approaches have been proposed. Investigations on the prediction of evolution have centered on monitoring disease activity. Disease activation biomarkers includeinterleukin-6, nitric oxide and nitric oxide synthase, osteopontin, and fetuin-A.[97] On the other hand since disease progression is the result of neurodegeneration the roles of proteins indicative of neuronal, axonal, and glial loss such as neurofilaments, tau and N-acetylaspartate are under investigation.[97] A final investigative field is work with biomarkers that distinguish between medication responders and nonresponders.[97]
The improvement in neuroimaging techniques such as positron emission tomography (PET) or magnetic resonance imaging (MRI) carry a promise for better diagnosis and prognosis predictions, albeit the effect of such improvements in daily medical practice may take several decades.[95] Regarding MRI, there are on the one hand several techniques that have already shown some usefulness in research settings and could be introduced into clinical practice, such as double-inversion recovery sequences, magnetization transfer, diffusion tensor, or functional magnetic resonance imaging.[98] These techniques have a higher pathological specificity than existing ones, but still lack some development including standarization of acquisition protocols and the creation of normative values.[98] On the other hand, there are also several techniques under development that could be useful.[98] These include the use of new contrast agents capable of measuring levels of peripheral macrophages, inflammation, or neuronal dysfunction.[98] Other techniques may quantify iron deposition and could serve to evaluate the role of this pathological feature in MS, or cerebral perfusion, which is known to be altered in patients.[98] Similary new PET radiotracers might serve as markers of altered proccessess in MS such as brain inflammation, cortical pathology,apoptosis, or remylienation.[99]
Clinical measures of evolution
The main measure of evolution of symptoms, specially important as an endpoint in MS trials, is the EDSS. However, this and other measures used in clinical studies are far from perfect and suffer from insetiveness or inadequate validation.[100] In this sense there is ongoing research to improve the EDSS and other measures such as the Multiple Sclerosis Functional Composite. This is specially important at the current state of research where the greater efficacy of existing medications force functional measures in clinical trials to be highly sensitive in order to adequately measure disease changes.[100]
Genetics
Progress in the field of genetics has been outstanding in the last two decades with highly improved methods and cheaper tests. These advances have in turn led to a greater understanding of the genetic component of MS. This trend is expected to continue, raising the possibility of discovering key mechanisms implicated in the disease. However, it is hard to predict how this future discoveries will impact in the clinical practice or in the research for new drugs and treatments.[95]
An example of a soon-to-be finished study is the Wellcome Trust case control consortium, a massive collaboration study including 120,000 genetic samples, of which 8000 are from individuals with MS.[18] This study may presummibly identify all the common genetic variants involved in MS.[18] Further studies will probably involve full genome sequencing of large samples, or the study of structural genetic variants such as insertions, deletions or polymorphisms.[18]
Drugs
Research directions on MS treatments include investigations of MS pathogenesis and heterogeneity; research of more effective, convenient, or tolerable new treatments for RRMS; creation of therapies for the progressive subtypes; neuroprotection strategies; and the search for effective symptomatic treatments.[101]
Advances during the last decades has led to the recent approval of several oral drugs. These drugs are expected to gain in popularity and frequency of use at the expense of previously existing therapies.[95] Further oral drugs are still under investigation, the most notable example being laquinimod, which was announced in August 2012 to be the focus of a third phase III trial after mixed results in the previous ones.[102] Similarly, Other studies are aimed to improve efficacy and ease of use of already existing therapies through the use of novel preparations. Such is the case the PEGylated version of interferon-β-1a, that has a longer life than normal interferon and therefore it is being studied if given at less frequent doses has a similar efficacy than the existing product.[103][104] Request for approval of peginterferon beta-1a is expected during 2013.[104]
Monoclonal antibodies, which are drugs of the same family as natalizumab, have also raised high levels of interest and research. Alemtuzumab,daclizumab and CD20 monoclonal antibodies such as rituximab, ocrelizumab and ofatumumab have all shown some benefit and are under study as potential treatments for MS.[105] Nevertheless their use has also been accompanied by the appearance of potentially dangerous adverse effects, most importantly opportunistic infections.[95] Related to these investigations is the recent development of a test against JC virus antibodies which might help to predict what patients are at a greater risk of developing progressive multifocal leukoencephalopathy when taking natalizumab.[95] While monoclonal antibodies are probably going to have some role in the treatment of the disease in the future, it is believed that it will be small due to the risks associated to them.[95]
Another research strategy is to evaluate the combined effectiveness of two or more drugs.[106] The main rationale for polytherapy in MS is that the involved treatments target different mechanisms of the disease and therefore their use is not necessarily exclusive.[106] Moreover synergies, in which a drug potentiates the effect of another are also possible. Nevertheless there can also appear important drawbacks such as antagonizing mechanisms of action or potentiation of deleterious secondary effects.[106] While there have been several clinical trials of combined therapy none has shown positive enough effects to merit the consideration as a viable treatment for MS.[106]
Finally, regarding neuroprotective and specially regenerative treatments, such as stem cell therapy, while their research is considered of high importance at the moment they are only a promise of future therapeutic approaches.[107] Likewise, there are not any effective treatments for the progressive variants of the disease. Many of the newest drugs as well as those under development are probably going to be evaluated as therapies for PPMS or SPMS, and their improved effectiveness when compared with previously existing drugs may eventually lead to a positive result in these groups of patients.[95]
Chronic cerebrospinal venous insufficiency
Main article: Chronic cerebrospinal venous insufficiency
In 2008, vascular surgeon Paolo Zamboni suggested that MS involves a vascular process he referred to as chronic cerebrospinal venous insufficiency (CCSVI), in which veins from the brain are constricted. He found CCSVI in all patients with MS in his study, performed a surgical procedure, later called in the media "liberation procedure" to correct it and claimed that 73% of participants improved.[108] This theory received important attention in the media and among MS patients, specially in Canada.[109] Concern has been raised with Zamboni's research as it was neither blinded nor controlled, and additionally its assumptions about the pathophisiology of the disease may not be backed by known data.[110] Also further studies have either not found a relationship or found a much less strong one.[111] This has raised serious objections to the hypothesis of CCSVI originating MS.[112] The "liberation procedure" has been criticized for possibly resulting in serious complications and deaths while its benefits have not been proven.[110] Currently it is recommended not to use the proposed treatment unless its effectiveness is confirmed by controlled studies.[113] Research on CCSVI has been fast tracked but researchers have been unable to confirm whether CCSVI has a role in causing MS.[111]
See also
References
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af agah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bcbd be bf bg Compston, A; Coles, A (2008 Oct 25). "Multiple sclerosis.". Lancet 372 (9648): 1502–17. PMID 18970977.
- ^ a b Rosati G (April 2001). "The prevalence of multiple sclerosis in the world: an update". Neurol. Sci. 22 (2): 117–39. doi:10.1007/s100720170011. PMID 11603614.
- ^ a b c Clanet M (June 2008). "Jean-Martin Charcot. 1825 to 1893" (PDF). Int MS J 15 (2): 59–61. PMID 18782501.
* Charcot, J. (1868). "Histologie de la sclerose en plaques".Gazette des hopitaux, Paris 41: 554–5. - ^ a b c d e f g h i j k l m n o p q Compston A, Coles A (April 2002). "Multiple sclerosis". Lancet 359 (9313): 1221–31.doi:10.1016/S0140-6736(02)08220-X. PMID 11955556.
- ^ a b c d e f g h Ascherio A, Munger KL (April 2007). "Environmental risk factors for multiple sclerosis. Part I: the role of infection". Ann. Neurol. 61 (4): 288–99.doi:10.1002/ana.21117. PMID 17444504.
- ^ Mazziotta, John C.; Robert I. Simon MD; Gerald Miletello MD; MD, Joseph Capella (2012). "Depression and Psychosis in Neurological Practice.". Bradley's Neurology in Clinical Practice: Expert Consult - Online and Print, 6e (Bradley, Neurology in Clinical Practice e-dition 2v Set). Philadelphia: Saunders. ISBN 1-4377-0434-4.
- ^ a b c d e f g h Lublin FD, Reingold SC (April 1996). "Defining the clinical course of multiple sclerosis: results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis". Neurology 46 (4): 907–11.doi:10.1212/WNL.46.4.907. PMID 8780061.
- ^ a b c Weinshenker BG (1994). "Natural history of multiple sclerosis". Ann. Neurol. 36 (Suppl): S6–11.doi:10.1002/ana.410360704. PMID 8017890.
- ^ Davis FA, Bergen D, Schauf C, McDonald I, Deutsch W (November 1976). "Movement phosphenes in optic neuritis: a new clinical sign". Neurology 26 (11): 1100–4.doi:10.1212/WNL.26.11.1100. PMID 988518.
- ^ Page NG, Bolger JP, Sanders MD (January 1982)."Auditory evoked phosphenes in optic nerve disease". J. Neurol. Neurosurg. Psychiatr. 45 (1): 7–12.doi:10.1136/jnnp.45.1.7. PMC 491258.PMID 7062073.
- ^ Kurtzke JF (1983). "Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS)". Neurology 33 (11): 1444–52.doi:10.1212/WNL.33.11.1444. PMID 6685237.
- ^ a b Tataru N, Vidal C, Decavel P, Berger E, Rumbach L (2006). "Limited impact of the summer heat wave in France (2003) on hospital admissions and relapses for multiple sclerosis". Neuroepidemiology 27 (1): 28–32.doi:10.1159/000094233. PMID 16804331.
- ^ Heesen C, Mohr DC, Huitinga I, et al. (March 2007). "Stress regulation in multiple sclerosis: current issues and concepts". Mult. Scler. 13 (2): 143–8.doi:10.1177/1352458506070772. PMID 17439878.
- ^ Martinelli V (2000). "Trauma, stress and multiple sclerosis". Neurol. Sci. 21 (4 Suppl 2): S849–52.doi:10.1007/s100720070024. PMID 11205361.
- ^ Minagar A, Jy W, Jimenez JJ, Alexander JS. (April 2006)."Multiple sclerosis as a vascular disease". Neurol Res.28 (3): 230–5. doi:10.1179/016164106X98080.PMID 16687046.
- ^ Dyment DA, Ebers GC, Sadovnick AD (February 2004). "Genetics of multiple sclerosis". Lancet Neurol 3 (92): 104–10. doi:10.1016/S1474-4422(03)00663-X.PMID 14747002.
- ^ "Who gets MS?". Multiple Sclerosis Trust. December 30, 2009. Retrieved April 18, 2011.
- ^ a b c d e f g Baranzini SE (June 2011). "Revealing the genetic basis of multiple sclerosis: are we there yet?".Curr. Opin. Genet. Dev. 21 (3): 317–24.doi:10.1016/j.gde.2010.12.006. PMC 3105160.PMID 21247752.
- ^ a b c d e f g h Marrie RA (December 2004). "Environmental risk factors in multiple sclerosis aetiology". Lancet Neurol 3(12): 709–18. doi:10.1016/S1474-4422(04)00933-0.PMID 15556803.
- ^ a b c d e Ascherio A, Munger KL (June 2007). "Environmental risk factors for multiple sclerosis. Part II: Noninfectious factors". Ann. Neurol. 61 (6): 504–13.doi:10.1002/ana.21141. PMID 17492755.
- ^ Ascherio A, Munger KL, Simon KC (June 2010). "Vitamin D and multiple sclerosis". Lancet Neurol 9 (6): 599–612.doi:10.1016/S1474-4422(10)70086-7. PMID 20494325.
- ^ Ghadirian P, Jain M, Ducic S, Shatenstein B, Morisset R (1998). "Nutritional factors in the aetiology of multiple sclerosis: a case-control study in Montreal, Canada". Int J Epidemiol. 27 (5): 845–52. doi:10.1093/ije/27.5.845.PMID 9839742. (primary source)
- ^ Spitsin S, Koprowski H (2008). "Role of uric acid in multiple sclerosis". Curr. Top. Microbiol. Immunol. Current Topics in Microbiology and Immunology 318: 325–42.doi:10.1007/978-3-540-73677-6_13. ISBN 978-3-540-73676-9. PMID 18219824.
- ^ a b c Kurtzke JF (October 1993). "Epidemiologic evidence for multiple sclerosis as an infection". Clin. Microbiol. Rev. 6 (4): 382–427. doi:10.1128/CMR.6.4.382.PMC 358295. PMID 8269393.
- ^ Gilden DH (March 2005). "Infectious causes of multiple sclerosis". The Lancet Neurology 4 (3): 195–202.doi:10.1016/S1474-4422(05)01017-3. PMID 15721830.
- ^ Ho,PP et al.; Kanter, J. L.; Johnson, A. M.; Srinagesh, H. K.; Chang, E.-J.; Purdy, T. M.; Van Haren, K.; Wikoff, W. R. et al. (2012). "Identification of naturally occurring fatty acids of the myelin sheath that resolve neuroinflammation". Science Translational Medicine 4 (137): 137–73.doi:10.1126/scitranslmed.3003831. PMID 22674551.
- ^ Wucherpfennig, K.; Strominger, J. (1995). "Molecular mimicry in T cell-mediated autoimmunity: Viral peptides activate human T cell clones specific for myelin basic protein". Cell 80 (5): 695–705. doi:10.1016/0092-8674(95)90348-8. PMID 7534214.
- ^ a b Chari DM (2007). "Remyelination in multiple sclerosis".Int. Rev. Neurobiol. International Review of Neurobiology 79: 589–620. doi:10.1016/S0074-7742(07)79026-8.ISBN 978-0-12-373736-6. PMID 17531860.
- ^ Pittock SJ, Lucchinetti CF (March 2007). "The pathology of MS: new insights and potential clinical applications".Neurologist 13 (2): 45–56.doi:10.1097/01.nrl.0000253065.31662.37.PMID 17351524.
- ^ Iglesias A, Bauer J, Litzenburger T, Schubart A, Linington C (November 2001). "T- and B-cell responses to myelin oligodendrocyte glycoprotein in experimental autoimmune encephalomyelitis and multiple sclerosis". Glia 36 (2): 220–34. doi:10.1002/glia.1111. PMID 11596130.
- ^ Trojano M, Paolicelli D (November 2001). "The differential diagnosis of multiple sclerosis: classification and clinical features of relapsing and progressive neurological syndromes". Neurol. Sci. 22 (Suppl 2): S98–102.doi:10.1007/s100720100044. PMID 11794488.
- ^ Poser CM, Brinar VV (June 2004). "Diagnostic criteria for multiple sclerosis: an historical review". Clin Neurol Neurosurg 106 (3): 147–58.doi:10.1016/j.clineuro.2004.02.004. PMID 15177763.
- ^ a b c d McDonald WI, Compston A, Edan G, et al. (July 2001). "Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis". Ann. Neurol. 50 (1): 121–7.doi:10.1002/ana.1032. PMID 11456302.
- ^ Polman CH, Reingold SC, Edan G, et al. (December 2005). "Diagnostic criteria for multiple sclerosis: 2005 revisions to the "McDonald Criteria"". Ann. Neurol. 58 (6): 840–6. doi:10.1002/ana.20703. PMID 16283615.
- ^ Rashid W, Miller DH (February 2008). "Recent advances in neuroimaging of multiple sclerosis". Semin Neurol 28 (1): 46–55. doi:10.1055/s-2007-1019127. PMID 18256986.
- ^ Link H, Huang YM (November 2006). "Oligoclonal bands in multiple sclerosis cerebrospinal fluid: an update on methodology and clinical usefulness". J. Neuroimmunol.180 (1–2): 17–28. doi:10.1016/j.jneuroim.2006.07.006.PMID 16945427.
- ^ Gronseth GS, Ashman EJ (May 2000). "Practice parameter: the usefulness of evoked potentials in identifying clinically silent lesions in patients with suspected multiple sclerosis (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology 54 (9): 1720–5.doi:10.1212/WNL.54.9.1720. PMID 10802774.
- ^ Pittock SJ, Rodriguez M (2008). "Benign multiple sclerosis: a distinct clinical entity with therapeutic implications". Curr. Top. Microbiol. Immunol. Current Topics in Microbiology and Immunology 318: 1–17. doi:10.1007/978-3-540-73677-6_1. ISBN 978-3-540-73676-9. PMID 18219812.
- ^ Feinstein, Anthony (2007). The clinical neuropsychiatry of multiple sclerosis (2nd ed. ed.). Cambridge: Cambridge University Press. p. 20. ISBN 052185234X.
- ^ a b Miller D, Barkhof F, Montalban X, Thompson A, Filippi M (May 2005). "Clinically isolated syndromes suggestive of multiple sclerosis, part I: natural history, pathogenesis, diagnosis, and prognosis". Lancet Neurol 4 (5): 281–8.doi:10.1016/S1474-4422(05)70071-5. PMID 15847841.
- ^ Rovaris M, Confavreux C, Furlan R, Kappos L, Comi G, Filippi M (April 2006). "Secondary progressive multiple sclerosis: current knowledge and future challenges". Lancet Neurol 5 (4): 343–54. doi:10.1016/S1474-4422(06)70410-0. PMID 16545751.
- ^ a b c Miller DH, Leary SM (October 2007). "Primary-progressive multiple sclerosis". Lancet Neurol 6 (10): 903–12. doi:10.1016/S1474-4422(07)70243-0.PMID 17884680.
- ^ Stadelmann C, Brück W (November 2004). "Lessons from the neuropathology of atypical forms of multiple sclerosis".Neurol. Sci. 25 (Suppl 4): S319–22. doi:10.1007/s10072-004-0333-1. PMID 15727225.
- ^ Burton, JM (2012 Dec 12). "Oral versus intravenous steroids for treatment of relapses in multiple sclerosis.".Cochrane Database of Systematic Reviews (12):CD006921 (Orig. rev.).doi:10.1002/14651858.CD006921. PMID 23235634.
- ^ Multiple sclerosis : national clinical guideline for diagnosis and management in primary and secondary care (pdf). London: Royal College of Physicians. 2004. pp. 54–57.ISBN 1-86016-182-0. PMID 21290636. Retrieved 6 February 2013.
- ^ a b "FDA approves first oral drug to reduce MS relapses"(Press release). US FDA. 2010-09-22. Retrieved 2013-01-21.
- ^ a b c "FDA approves new multiple sclerosis treatment Aubagio" (Press release). US FDA. 2012-09-12. Retrieved 2013-01-21.
- ^ a b c d e "Biogen Idec’s TECFIDERA™ (Dimethyl Fumarate) Approved in US as a First-Line Oral Treatment for Multiple Sclerosis". Biogen Idec Press Release. 2013-03-27.
- ^ "NDA 204063 - FDA Approved Labeling Text". US Food and Drug Agency. 27 March 2013. Retrieved 5 April 2013.
"NDA Approval". US Food and Drug Agency. 27 March 2013. Retrieved 5 April 2013. - ^ Natalizumab Injection. US National Library of Medicine (Medline) (2006-10-01). Retrieved on 2007-09-02.
- ^ Marriott, J. J.; Miyasaki, J. M.; Gronseth, G.; O'Connor, P. W. (3 May 2010). "Evidence Report: The efficacy and safety of mitoxantrone (Novantrone) in the treatment of multiple sclerosis: Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology". Neurology 74 (18): 1463–1470.doi:10.1212/WNL.0b013e3181dc1ae0. PMC 2871006.PMID 20439849.
- ^ Kappos, L; Bates, D; Edan, G; Eraksoy, M; Garcia-Merino, A; Grigoriadis, N; Hartung, HP; Havrdová, E; Hillert, J; Hohlfeld, R; Kremenchutzky, M; Lyon-Caen, O; Miller, A; Pozzilli, C; Ravnborg, M; Saida, T; Sindic, C; Vass, K; Clifford, DB; Hauser, S; Major, EO; O'Connor, PW; Weiner, HL; Clanet, M; Gold, R; Hirsch, HH; Radü, EW; Sørensen, PS; King, J (2011 Aug). "Natalizumab treatment for multiple sclerosis: updated recommendations for patient selection and monitoring". Lancet neurology 10 (8): 745–58.doi:10.1016/S1474-4422(11)70149-1. PMID 21777829.
- ^ Gylenya medication guide (pdf). Novartis Pharmaceuticals Corporation. May 2012. p. 2. Retrieved 2013-01-21.
- ^ He, D; Xu, Z; Dong, S; Zhang, H; Zhou, H; Wang, L; Zhang, S (2012 Dec 12). "Teriflunomide for multiple sclerosis". In Zhou, Hongyu. Cochrane database of systematic reviews (Online) 12: CD009882.doi:10.1002/14651858.CD009882.pub2.PMID 23235682.
- ^ Johnson KP (2007). "Control of multiple sclerosis relapses with immunomodulating agents". J. Neurol. Sci.256 (Suppl 1): S23–8. doi:10.1016/j.jns.2007.01.060.PMID 17350652.
- ^ a b c Comi G (October 2009). "Treatment of multiple sclerosis: role of natalizumab". Neurol. Sci. 30. Suppl 2 (S2): S155–8. doi:10.1007/s10072-009-0147-2.PMID 19882365.
- ^ a b Freedman, M. S. (27 December 2010). "Long-term follow-up of clinical trials of multiple sclerosis therapies".Neurology 76 (1, Supplement 1): S26–S34.doi:10.1212/WNL.0b013e318205051d.PMID 21205679.
- ^ Qizilbash, N; Mendez, I; Sanchez-de la Rosa, R (2012 Jan). "Benefit-risk analysis of glatiramer acetate for relapsing-remitting and clinically isolated syndrome multiple sclerosis". Clinical therapeutics 34 (1): 159–176.e5.doi:10.1016/j.clinthera.2011.12.006. PMID 22284996.
- ^ Bates, D (2011 Jan 4). "Treatment effects of immunomodulatory therapies at different stages of multiple sclerosis in short-term trials". Neurology 76 (1 Suppl 1): S14–25. doi:10.1212/WNL.0b013e3182050388.PMID 21205678.
- ^ Martinelli Boneschi F, Rovaris M, Capra R, Comi G (2005). "Mitoxantrone for multiple sclerosis". In Martinelli Boneschi, Filippo. Cochrane database of systematic reviews (Online)(4): CD002127. doi:10.1002/14651858.CD002127.pub2.PMID 16235298.
- ^ Leary SM, Thompson AJ (2005). "Primary progressive multiple sclerosis: current and future treatment options".CNS Drugs 19 (5): 369–76. doi:10.2165/00023210-200519050-00001. PMID 15907149.
- ^ Johnston, J; So, TY (2012 Jun 18). "First-line disease-modifying therapies in paediatric multiple sclerosis: a comprehensive overview". Drugs 72 (9): 1195–211.doi:10.2165/11634010-000000000-00000.PMID 22642799.
- ^ Sládková T, Kostolanský F (2006). "The role of cytokines in the immune response to influenza A virus infection". Acta Virol. 50 (3): 151–62. PMID 17131933.
- ^ Munari L, Lovati R, Boiko A (2004). "Therapy with glatiramer acetate for multiple sclerosis". In Munari, Luca M.Cochrane database of systematic reviews (Online) (1): CD004678. doi:10.1002/14651858.CD004678.PMID 14974077.
- ^ Tremlett H, Oger J (November 2004). "Hepatic injury, liver monitoring and the beta-interferons for multiple sclerosis".J. Neurol. 251 (11): 1297–303. doi:10.1007/s00415-004-0619-5. PMID 15592724.
- ^ a b Killestein, Joep; Rudick, Richard A; Polman, Chris H (1 November 2011). "Oral treatment for multiple sclerosis". The Lancet Neurology 10 (11): 1026–1034. doi:10.1016/S1474-4422(11)70228-9. PMID 22014437.
- ^ Kesselring J, Beer S (2005). "Symptomatic therapy and neurorehabilitation in multiple sclerosis". The Lancet Neurology 4 (10): 643–52. doi:10.1016/S1474-4422(05)70193-9. PMID 16168933.
- ^ Khan F, Turner-Stokes L, Ng L, Kilpatrick T (2007). "Multidisciplinary rehabilitation for adults with multiple sclerosis". In Khan, Fary. Cochrane Database Syst Rev (2): CD006036. doi:10.1002/14651858.CD006036.pub2.PMID 17443610.
- ^ a b Steultjens EM, Dekker J, Bouter LM, Leemrijse CJ, van den Ende CH (2005). "Evidence of the efficacy of occupational therapy in different conditions: an overview of systematic reviews". Clinical rehabilitation 19 (3): 247–54.doi:10.1191/0269215505cr870oa. PMID 15859525.
- ^ Steultjens EM, Dekker J, Bouter LM, Cardol M, Van de Nes JC, Van den Ende CH (2003). "Occupational therapy for multiple sclerosis". In Steultjens, Esther EMJ. Cochrane database of systematic reviews (Online) (3): CD003608.doi:10.1002/14651858.CD003608. PMID 12917976.
- ^ Gallien P, Nicolas B, Robineau S, Pétrilli S, Houedakor J, Durufle A (2007). "Physical training and multiple sclerosis".Ann Readapt Med Phys 50 (6): 373–6, 369–72.doi:10.1016/j.annrmp.2007.04.004. PMID 17482708.
- ^ Rietberg MB, Brooks D, Uitdehaag BMJ, Kwakkel G (2005). "Exercise therapy for multiple sclerosis". In Kwakkel, Gert.Cochrane Database of Systematic Reviews (1): CD003980.doi:10.1002/14651858.CD003980.pub2.PMID 15674920.
- ^ Thomas PW, Thomas S, Hillier C, Galvin K, Baker R (2006). "Psychological interventions for multiple sclerosis". In Thomas, Peter W. Cochrane Database of Systematic Reviews (1): CD004431.doi:10.1002/14651858.CD004431.pub2.PMID 16437487.
- ^ Mathiowetz V, Matuska KM, Murphy ME (2001). "Efficacy of an energy conservation course for persons with multiple sclerosis". Arch Phys Med Rehabil 82 (4): 449–56.doi:10.1053/apmr.2001.22192. PMID 11295003.
- ^ a b c d e f g Huntley A (January 2006). "A review of the evidence for efficacy of complementary and alternative medicines in MS". Int MS J 13 (1): 5–12, 4.PMID 16420779.
- ^ Olsen SA (2009). "A review of complementary and alternative medicine (CAM) by people with multiple sclerosis". Occup Ther Int 16 (1): 57–70.doi:10.1002/oti.266. PMID 19222053.
- ^ Farinotti M, Simi S, Di Pietrantonj C, et al. (2007). "Dietary interventions for multiple sclerosis". In Farinotti, Mariangela.Cochrane database of systematic reviews (Online) (1): CD004192. doi:10.1002/14651858.CD004192.pub2.PMID 17253500.
- ^ Chong MS, Wolff K, Wise K, Tanton C, Winstock A, Silber E (2006). "Cannabis use in patients with multiple sclerosis".Mult. Scler. 12 (5): 646–51.doi:10.1177/1352458506070947. PMID 17086912.
- ^ Bennett M, Heard R (2004). "Hyperbaric oxygen therapy for multiple sclerosis". In Bennett, Michael H. Cochrane database of systematic reviews (Online) (1): CD003057.doi:10.1002/14651858.CD003057.pub2.PMID 14974004.
- ^ Adams, Tim (23 May 2010). "Gut instinct: the miracle of the parasitic hookworm". The Observer.
- ^ a b c Phadke JG (May 1987). "Survival pattern and cause of death in patients with multiple sclerosis: results from an epidemiological survey in north east Scotland". J. Neurol. Neurosurg. Psychiatr. 50 (5): 523–31.doi:10.1136/jnnp.50.5.523. PMC 1031962.PMID 3495637.
- ^ Myhr KM, Riise T, Vedeler C, et al (February 2001)."Disability and prognosis in multiple sclerosis: demographic and clinical variables important for the ability to walk and awarding of disability pension". Mult. Scler. 7(1): 59–65. PMID 11321195.
- ^ a b c Alonso A, Hernán MA (July 2008). "Temporal trends in the incidence of multiple sclerosis: a systematic review".Neurology 71 (2): 129–35.doi:10.1212/01.wnl.0000316802.35974.34.PMID 18606967.
- ^ Multiple Sclerosis Fact Sheet CDC medical records on VoxHealth. Retrieved on 2013-30-1
- ^ Pugliatti, M; Sotgiu, S, Rosati, G (2002 Jul). "The worldwide prevalence of multiple sclerosis". Clinical neurology and neurosurgery 104 (3): 182–91. doi:10.1016/S0303-8467(02)00036-7. PMID 12127652.
- ^ Kulie T, Groff A, Redmer J, Hounshell J, Schrager S (2009). "Vitamin D: an evidence-based review". J Am Board Fam Med 22 (6): 698–706.doi:10.3122/jabfm.2009.06.090037. PMID 19897699.
- ^ a b Compston A (October 1988). "The 150th anniversary of the first depiction of the lesions of multiple sclerosis". J. Neurol. Neurosurg. Psychiatr. 51 (10): 1249–52.doi:10.1136/jnnp.51.10.1249. PMC 1032909.PMID 3066846.
- ^ Lassmann H (1999-10-29). "The pathology of multiple sclerosis and its evolution". Philos Trans R Soc Lond B Biol Sci. 354 (1390): 1635–40.doi:10.1098/rstb.1999.0508. PMC 1692680.PMID 10603616.
- ^ Lassmann H (July 2005). "Multiple sclerosis pathology: evolution of pathogenetic concepts". Brain Pathology 15 (3): 217–22. doi:10.1111/j.1750-3639.2005.tb00523.x.PMID 16196388.
- ^ Medaer R (September 1979). "Does the history of multiple sclerosis go back as far as the 14th century?". Acta Neurol. Scand. 60 (3): 189–92. doi:10.1111/j.1600-0447.1979.tb08970.x. PMID 390966.
- ^ Holmøy T (2006). "A Norse contribution to the history of neurological diseases". Eur. Neurol. 55 (1): 57–8.doi:10.1159/000091431. PMID 16479124.
- ^ Firth, D (1948). The Case of August D`Esté. Cambridge: Cambridge University Press.
- ^ a b Pearce JM (2005). "Historical descriptions of multiple sclerosis". Eur. Neurol. 54 (1): 49–53.doi:10.1159/000087387. PMID 16103678.
- ^ Barbellion, Wilhelm Nero Pilate (1919). The Journal of a Disappointed Man. New York: George H. Doran. ISBN 0-7012-1906-8.
- ^ a b c d e f g h i j Miller AE (2011). "Multiple sclerosis: where will we be in 2020?". Mt. Sinai J. Med. 78 (2): 268–79.doi:10.1002/msj.20242. PMID 21425270.
- ^ Mehta V, Pei W, Yang G, et al. (2013). "Iron is a sensitive biomarker for inflammation in multiple sclerosis lesions".PLoS ONE 8 (3): e57573.doi:10.1371/journal.pone.0057573. PMC 3597727.PMID 23516409.
- ^ a b c d Harris VK, Sadiq SA (2009). "Disease biomarkers in multiple sclerosis: potential for use in therapeutic decision making". Mol Diagn Ther 13 (4): 225–44.doi:10.2165/11313470-000000000-00000.PMID 19712003.
- ^ a b c d e Filippi M, Rocca MA, De Stefano N, et al.(December 2011). "Magnetic resonance techniques in multiple sclerosis: the present and the future". Arch. Neurol.68 (12): 1514–20. doi:10.1001/archneurol.2011.914.PMID 22159052.
- ^ Kiferle L, Politis M, Muraro PA, Piccini P (February 2011). "Positron emission tomography imaging in multiple sclerosis-current status and future applications". Eur. J. Neurol. 18 (2): 226–31. doi:10.1111/j.1468-1331.2010.03154.x. PMID 20636368.
- ^ a b Cohen JA, Reingold SC, Polman CH, Wolinsky JS (May 2012). "Disability outcome measures in multiple sclerosis clinical trials: current status and future prospects". Lancet Neurol 11 (5): 467–76. doi:10.1016/S1474-4422(12)70059-5. PMID 22516081.
- ^ Cohen JA (July 2009). "Emerging therapies for relapsing multiple sclerosis". Arch. Neurol. 66 (7): 821–8.doi:10.1001/archneurol.2009.104. PMID 19597083.
- ^ Jeffrey, susan (09 Aug 2012). "CONCERTO: A Third Phase 3 Trial for Laquinimod in MS". Medscape Medical News. Retrieved 21 May 2013.
- ^ Kieseier BC, Calabresi PA (March 2012). "PEGylation of interferon-β-1a: a promising strategy in multiple sclerosis".CNS Drugs 26 (3): 205–14. doi:10.2165/11596970-000000000-00000. PMID 22201341.
- ^ a b Biogen Idec (24 Jan 2013). "Biogen Idec Announces Positive Top-Line Results from Phase 3 Study of Peginterferon Beta-1a in Multiple Sclerosis-Press release". Retrieved 21 May 2013.
- ^ Saidha S, Eckstein C, Calabresi PA (January 2012). "New and emerging disease modifying therapies for multiple sclerosis". Ann. N. Y. Acad. Sci. 1247: 117–37.doi:10.1111/j.1749-6632.2011.06272.x.PMID 22224673.
- ^ a b c d Milo R, Panitch H (February 2011). "Combination therapy in multiple sclerosis". J. Neuroimmunol. 231 (1-2): 23–31. doi:10.1016/j.jneuroim.2010.10.021.PMID 21111490.
- ^ Luessi F, Siffrin V, Zipp F (September 2012)."Neurodegeneration in multiple sclerosis: novel treatment strategies". Expert Rev Neurother 12 (9): 1061–76; quiz 1077. doi:10.1586/ern.12.59. PMID 23039386.
- ^ Zamboni P, Galeotti R, Menegatti E, et al. (April 2009)."Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis". J. Neurol. Neurosurg. Psychiatr. 80(4): 392–9. doi:10.1136/jnnp.2008.157164.PMC 2647682. PMID 19060024.
- ^ Pullman D, Zarzeczny A, Picard A (2013). "Media, politics and science policy: MS and evidence from the CCSVI Trenches". BMC Med Ethics 14: 6. doi:10.1186/1472-6939-14-6. PMC 3575396. PMID 23402260.
- ^ a b Qiu J (May 2010). "Venous abnormalities and multiple sclerosis: another breakthrough claim?". Lancet Neurol 9(5): 464–5. doi:10.1016/S1474-4422(10)70098-3.PMID 20398855.
- ^ a b Ghezzi A, Comi G, Federico A (February 2011). "Chronic cerebro-spinal venous insufficiency (CCSVI) and multiple sclerosis". Neurol. Sci. 32 (1): 17–21. doi:10.1007/s10072-010-0458-3. PMID 21161309.
- ^ Dorne H, Zaidat OO, Fiorella D, Hirsch J, Prestigiacomo C, Albuquerque F, Tarr RW. (October 2010). "Chronic cerebrospinal venous insufficiency and the doubtful promise of an endovascular treatment for multiple sclerosis". J NeuroIntervent Surg 2 (4): 309–311.doi:10.1136/jnis.2010.003947. PMID 21990639.
- ^ Khan O, Filippi M, Freedman MS, Barkhof F, Dore-Duffy P, Lassmann H, Trapp B, Bar-Or A, Zak I, Siegel MJ, Lisak R (2010-02-12). "Chronic cerebrospinal venous insufficiency and multiple sclerosis". Annals of neurology (Annals of Neurology) 67 (3): 286–90. doi:10.1002/ana.22001.PMID 20373339.












Hello everyone, i'm Linda Harry from United State i was diagnosed with Parkinson Disease for over 6 years which made me loose my job and my relationship with my Fiance after he discovered that i was having Parkinson, he departed from me, and i tried all my best to make him stays, but he neglected me until a friend of mine from UK told me Great healer, who will restore my life back with his powerful healing herbal medicine. then he sent me his email address to contact him- drimolaherbalmademedicine@gmail.com. and i quickly contacted him, and he said my condition can be solved, that he will treat the disease immediately only if i can accept trust on him and accept his terms and condition, i Agreed because i was so much in need of help by all means, so i did all he instructed me to do. And surprisingly after two weeks, He sent me a text, that i should hurry up to the hospital for a checkup, which i truly did, i confirm from my doctor that i am now ( PARKINSON NEGATIVE) my eyes filled with tears and joy, crying heavily because truly the disease deprived me of many things from my life, This is a Miracle, dr imoloa also uses his powerful herbal medicine to cure the following diseases: lupus disease, mouth ulcer, mouth cancer, body pain, fever, hepatitis A.B.C., syphilis, diarrhea, HIV/AIDS, Huntington's Disease, back acne, Chronic renal failure, addison disease, Chronic Pain, Crohn's Disease, Cystic Fibrosis, Fibromyalgia, Inflammatory Bowel Disease, fungal nail disease, Lyme Disease, Celia disease, Lymphoma, Major Depression, Malignant Melanoma, Mania, Melorheostosis, Meniere's Disease, Mucopolysaccharidosis , Multiple Sclerosis, Muscular Dystrophy, Rheumatoid Arthritis, Alzheimer's Disease, parkison disease, vaginal cancer, epilepsy, Anxiety Disorders, Autoimmune Disease, Back Pain, Back Sprain, Bipolar Disorder, Brain Tumour, Malignant, Bruxism, Bulimia, Cervical Disk Disease, cardiovascular disease, Neoplasms, chronic respiratory disease, mental and behavioural disorder, Cystic Fibrosis, Hypertension, Diabetes, asthma, Inflammatory autoimmune-mediated arthritis. chronic kidney disease, inflammatory joint disease, impotence, feta alcohol spectrum, Dysthymic Disorder, Eczema, tuberculosis, Chronic Fatigue Syndrome, constipation, inflammatory bowel disease, bone cancer, lung cancer. contact him on email- drimolaherbalmademedicine@gmail.com. and also on whatssap- +2347081986098
ReplyDelete