Sunday, December 30, 2012
Funny things from today's CNA class
Funny things from today's CNA class
Raised big cats for the zoo
Have a hyperdilated pupil (from stroke)
Seen a classmates brain (was an OR tech when the student with the hyperdilated eye had a stroke)
Was doing a paper route and found someone hanging from a tree (suicide)
A car crashed into my house and landed on my bed (I wasn't in it)
My husband and I ran away from the FLDS church
Felt my c-section
Was tricked into eating poo
Met my husband riding bulls
Friday, December 28, 2012
CNA Training Blood PressuresPP
UTAH CNA CLASS
At clinical there was a group of female residents sitting around the dining room table. One of our male students approached the group and asked "how are you ladies doing?" One of them responded "we are doing great. We are planning our future with you!"
VIRTUAL DAY AT CNA SCHOOL
 |
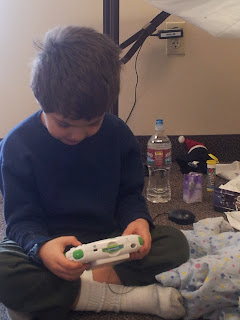
| My kiddo was sick so he came to CNA class with me. Brought his Christmas toys. |
 |
| Vita answering phone calls at CNA class |
 |
| Hmm, not working very hard at CNA class |
 |
| Doing something with the mannequin while reading their CNA skill sbook |
 |
| Checking for pressure sores |
 |
| Getting those straps on right on the hoyer lift |
 |
| Away she goes |
 |
| Doing a little mannequin repair at CNA class |
 |
| How many CNA students does it take to repair a mannequin? |
Wednesday, December 26, 2012
Utah CNA clinical
We are at Avalon doing clinical today. It's snowy outside and getting here was an adventure for some of the students, particullarly the ones from Payson and Park City,
I just asked a resident on the Valley Mental Health side if she was going to breakfast, she sneered at me and asked "what are you writing a book?"
Hm, well maybe I will.
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
I just asked a resident on the Valley Mental Health side if she was going to breakfast, she sneered at me and asked "what are you writing a book?"
Hm, well maybe I will.
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
TWO WEEK UTAH CNA CLASS
Saturday, December 22, 2012
UTAH CNA CLINICAL
It was a little slow at clinical so we did hand massages, nails and one of the students even played the piano. A good time was had by all:)
 |
| entertaining the residents at clinical |
 |
| Showing a little love to the residents at clinical |
 |
| I think I love you! |
 |
| Hand massages at CNA clinical |
 |
| Manicures for everyone |
Tuesday, December 18, 2012
CNA Game
In today's get to know each other game here were some of our unique things:
Linguist speak 13 languages
Have over 55 pair of shoes
Paid to have fish eat my feet in Jerusalem
Tested out of High School
Ate 10 pounds of ice cream in 30 minutes
Write in a different font every semester
Rodeo Queen 8 times
Utah nursing homes see fewer serious problems than nation

Utah nursing homes see fewer serious problems than nation
Inspections • The facilities get among the lowest average fines.
By heather may
The Salt Lake Tribune
Published: December 17, 2012 12:21PMUpdated: December 17, 2012 10:55PM
DDuring an inspection of a nursing home in Ogden last year, state regulators found three residents who were in “immediate jeopardy.”
One resident at Mountain View Health Services who needed a feeding tube was fed while he was lying down. Food had entered his airway in the past but he continued to be fed in that position. He had developed aspiration pneumonias five times and became bed-bound. Inspectors reviewed medical notes and could see no evidence that the facility had tried to prevent the problems, and they personally witnessed improper feedings five times.
Two other residents were found to have fallen dozens of times — one fell 49 times in a year, with a handful resulting in serious injuries including a skull fracture — but the facility hadn’t made changes to prevent further tumbles, according to the inspection report.
Those are two of some of the most serious deficiencies cited at eight of Utah’s 88 nursing homes. At least one, Orem Rehabilitation and Nursing Center, was cited in a death, after staff members failed to use a suction machine to clear a patient’s airway.
The reports are available on the Nursing Home Inspect tool created by the nonprofit news organization ProPublica. The investigative newsroom took publicly available inspection reports and created an app that makes them more user-friendly, with state-specific pages listing nursing homes and their inspection reports. It also linked the reports to federal fines and other sanctions taken against the homes, revealing wide disparities between states.
The app, available to the public at http://projects.propublica.org/nursing-homes, shows Utah nursing homes have some of the fewest serious deficiencies per home. The state also has some of the country’s lowest average fines, at $2,500 compared to the highest in Washington at $90,000, and one of the lowest number of payment suspensions. That is when the federal Centers for Medicaid and Medicare (CMS) refuses to pay for new patient admissions.
Utah had two payment suspensions in the past three years, compared to Texas’ 198.
The Utah Department of Health, which inspects the homes for CMS, said it wasn’t keeping fines low. It follows guidelines on civil-penalty amounts issued by the regional CMS office, said Greg Bateman, manager of long-term care surveys.
CMS can overrule what local inspectors suggest, he said. Within the six-state region, Utah is one of two states that levied fines. Montana, North Dakota, South Dakota and Wyoming didn’t, according to the ProPublica data.
Utah’s two payment suspensions took place at Deseret Care Center, Salt Lake City, and Four Corners Regional Care Center, Blanding, both this past summer.
Inspection reports note that Four Corners didn’t notify two patients’ physicians when they were injured, and it didn’t assess a patient who complained of abdominal pain. The patient later insisted on going to the hospital. Another patient wasn’t sent to the hospital after complaining about rib pain.
Deseret Care was faulted for 27 deficiencies this summer, including dirty conditions such as rooms that strongly smelled of urine, not cleaning a resident who had been incontinent, leaving patients in pain or confusion because the facility didn’t have their prescribed medication, and not investigating an incident in which a resident called another resident the “N-word” and hit her with his walker.
The website allows users to find facilities with the highest and lowest number of deficiencies and fines.
Mountain View Health had Utah’s highest number of total deficiencies, at 101, and highest number of serious ones — in which residents are in immediate jeopardy — at four. It has also been fined the most amount, nearly $28,000.
“It caught us all completely off guard,” Mountain View administrator Reece Nelson said of the poor inspection. “It wasn’t really an accurate picture of what this facility is all about.”
He said the facility improved its system for preventing falls and trained employees on feeding patients who use a gastrostomy tube.
“Our focus,” he said, “certainly is the safety and the care of our residents.”
—
Citations in Utah
These Utah nursing homes were cited for serious deficiencies, according to three years of data compiled by ProPublica.
Patient death
Orem Rehabilitation and Nursing Center was cited Sept. 12, 2011, in connection with a patient death, for not providing necessary care.
The patient, who struggled to breathe and couldn’t swallow, was fed a drink and solid food. When her breathing worsened, no CPR was performed because she had a Do Not Resuscitate order, and she died.
However, staff were supposed to use suction for her medical condition, which was not disclosed. Staff later said they didn’t know where the facilities’ emergency equipment was located or if it included a suction machine. The director of nursing later said she had not done any emergency-preparedness training with the staff in the past year she was there.
Patient injuries and risks
Aspen Ridge Transitional Rehab, Murray, cited Sept. 22, 2010,for not preventing avoidable accidents. Hand-sink temperatures were as high as 146.5 F.
Canyon Rim Care Center, Salt Lake City, cited June 21 for not preventing avoidable accidents. Windows in two rooms on the third floor opened the full length but should only open six inches.
Deseret Care Center, Salt Lake City, cited July 15, 2010, for not preventing avoidable accidents. Hand-sink temperatures were as high as 140 degrees.
Provo Rehabilitation and Nursing, cited Feb. 2for not keeping residents safe from serious medication errors. Patients were given more insulin than ordered by their physicians.
Rocky Mountain Care, Murray, cited Aug. 19, 2009, for not protecting residents from abuse. Staff members used physical force to bring a resident into the building, place him in bed and take his wheelchair against his will.
Thatcher Brook Rehabilitation and Care, Clearfield, cited July 6, 2010, for not preventing avoidable accidents. Hand-sink temperatures were as high as 125. A patient had complained, but no action was taken.
Source: ProPublica
© Copyright 2012 The Salt Lake Tribune. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
Utah nursing homes see fewer serious problems than nation
By heather may
The Salt Lake Tribune
Layton students make 1,000 cranes for kids at Primary Children’s

Layton students make 1,000 cranes for kids at Primary Children’s
Parent involvement • Tomoko Hauck donated origami paper and taught classes how to fold the birds.
By Carol Lindsay
Special to The Tribune
Published: December 17, 2012 01:25PMUpdated: December 17, 2012 01:25PM
Carol Lindsay | Special to The Tribune Students at Layton's Ellison Park Elementary make origami cranes to give to patients at Primary Children's Medical Center over the holidays.
Layton • Children are talking, fingers are fumbling and paper is folding as second graders struggle to create origami cranes in April Moss’ second grade class.
Students are learning about the Japanese legend of a thousand origami cranes. The legend says if a person makes 1,000 origami paper cranes and strings them together, the creator will be granted a wish. Because of this legend, origami cranes are a popular gift in Japan.
Tomoko Hauck, a mother of students at Ellison Park Elementary in Layton, is sharing her origami skills with the students. Hauck offered to teach participating classes how to make origami cranes. Hauck’s goal is to make 1,000 cranes and present them to children at Primary Children’s Medical Center during the holiday season.
“I’m from Japan, and the culture in Japan is we make cranes for the sick to get better. The person who makes the cranes is granted a promise and we want to do this for the children in Salt Lake City,” Hauck said.
Hauck has made cranes for children in her community before but she had never included the school.
Vice Principal Eve Bean was thrilled with the undertaking.
“Any time we have a service learning experience in the classroom it strengthens the learning. The children can apply the skill while at the same time doing something good,” she said. “Mrs. Hauck is a very giving person. Not only has she given her time and talent, but she has also donated all the paper for the cranes.”
The project was open to all the school’s teachers, who decided whether the activity was appropriate for their students and whether they wanted to integrate it into their schedule. About 320 children at the school are participating in the project.
Ellison Park elementary has had several students treated at Primary Children’s hospital, so the experience is a personal one for students. When second grade teacher April Moss asked her students what they would wish for the children in the hospital one student replied “that they get their hair back.” Another student responded, “No one cares if they are bald; we just want them to be healthy.”
A patient instructor, Hauck taught a class of 25 seven-year-olds to fold the cranes one step at a time as they clamored around her. Some of the boys became distracted when the incomplete crane took on the form of a space ship and a few cranes took flight. Another child put her head on the desk, declaring “It’s too hard!”
The students, though, continue to work on their creations.
“If your crane breaks you have to start over,” said Hailey Gardula.
And they are keeping their goal in mind despite the occasional frustration. Before Christmas, Hauck along with teachers from the school and the student council will go to Primary Children’s Hospital and present their gift.
“It’s fun to make cranes,” said second grader Mason Padilla. “I like to make things and fold things and it is going to make the children in the hospital happy.”
closeup@sltrib.com
Twitter: @sltribDavis
© Copyright 2012 The Salt Lake Tribune. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
Layton students make 1,000 cranes for kids at Primary Children’s
By Carol Lindsay
Special to The Tribune
Monday, December 17, 2012
UNAR AGAIN CNA TEST
Please replace any mention of ‘Universal Precautions’ or ‘Body Substance Isolation’ to Standard Precautions. It has been changed in the handbook that is online and is also listed on the State Skills testing sheet for skills examiners, so PLEASE RELAY TO YOUR STUDENTS AND ALL INSTRUCTORS
UTAH CNA CLASSES
UTAH CNA CLASSES
UNAR wants you to know
Please teach your students:
1. Do not clip toenails. Nurses or podiatrists do all diabetic nails. May clip fingernails.
MAKE SURE YOUR STUDENTS ARE AWARE OF THIS INFORMATION, WHICH IS IN THE CANDIDATE HANDBOOK:
All testing sites comply with the ADA (American Disabilities Act) [42U.S.C. § 12101 et seq] and all other documented disabilities. If you have a disability or require an accommodation, you will need to make arrangements with the testing center when you call for your testing appointment.
1. The written examination is offered online at a designated testing site.
2. It is also available in audio, where the candidate can have headphones, and listen and read at the same time. All testing sites must have this available. The test sites would like to know this in advance.
3. If a candidate has a 504, ADA disability, is with Vocational Rehab or in a Special Education class in High School, they may have a reader from the testing site. They cannot bring their own reader. This must be available at all sites.
4. A paper and pencil test is available if you are granted an accommodation. The paper test must be ordered in advance. Prior notification to test site is required.
5. The candidate is not allowed to have a foreign language interpreter.
6. A candidate may use a translation dictionary in their native language, (not a definition dictionary); only after the test center proctor has checked the dictionary for notes and verified that it is a translation-only dictionary. (Please allow the test center time to review the dictionary)
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
UTAH CNA CLASSES
UTAH CNA SCHOOLS
UTAH CNA TRAINING
UTAH CNA EDUCATION
Sunday, December 16, 2012
St Joseph's Villa Mass
Nope, the residents did not have tags on their wheelchairs. There were lots of people from the community at mass. There was even a priest and nun who were residents at the facility. The priest did a very nice service. He was young and enthusiastic, feel joy and share were his take aways. I appreciated that he talked about the tragedies in Connecticut this week. They didn't mention it at the service I went to earlier in the day and I was thinking about it as I'm sure were others.
Somebody was giving a resident a drink of water and the nun jumped up to tell her to stop. I've never seen a nun move so fast.
It really was a beautiful service.
Somebody was giving a resident a drink of water and the nun jumped up to tell her to stop. I've never seen a nun move so fast.
It really was a beautiful service.
The Secrets of Aging Well.
Live Long and Prosper
If fighting off Father Time by deflating your cholesterol count and stress levels is tucked somewhere in the back of your mind, maybe you should keep it there. With a longer, healthier life as a goal, perhaps you should be turning more of your attention to making friends, waging war on your waistline, and extinguishing your cigarettes for good.
That is some of the wisdom emerging from the Harvard Study of Adult Development, the longest, most comprehensive examination of aging ever conducted. Since the 1930s, researchers have studied more than 800 men and women, following them from adolescence into old age, and seeking clues to the behaviors that translate into happy and healthy longevity.
The results haven't always been what even the investigators themselves anticipated. "I had expected that the longevity of your parents, the quality of your childhood, and your cholesterol levels would be very influential," says psychiatrist George Vaillant, MD, director of the Harvard study and senior physician at Brigham and Women's Hospital in Boston. "So I was very surprised that these particular variables weren't more important than they were."
Surprisingly, stressful events didn't predict future health, either. "Some people had a lot of stress, but aged very well," says Vaillant. "But how you deal with that stress does matter quite a bit."
In fact, rather than obsessing about your cholesterol, or even the genetic hand you were dealt, the Harvard study found that you'd be better off becoming preoccupied with the following factors that turned out to be most predictive of whether you'd move successfully through middle age and into your 80s:
- Avoiding cigarettes
- Good adjustment or coping skills ("making lemonade out of lemons")
- Keeping a healthy weight
- Exercising regularly
- Maintaining strong social relationships (including a stablemarriage)
- Pursuing education
Woody Allen once observed that no one gets out of this world alive, but for as long as we're here, says Vaillant, we might as well stay as healthy and happy as possible. Vaillant, whose book Aging Well describes the decades-long Harvard study, says that it's "astonishing how many of the ingredients that predict longevity are within your control."
You've Gotta Have Friends
Aging successfully, according to Vaillant, is something like being tickled -- it's best achieved with another person. Whether your social connections are with a spouse, offspring, siblings, bridge partners, and/or fellow churchgoers, they're crucial to good health while growing older.
Richard Lucky, one of the so-called "happy-well" participants in the Harvard study, was always surrounded by people, whether it was having friends over for dinner or interacting with his children and grandchildren. In his 70s, he sailed with his wife from San Francisco to Bali, and he had begun writing a book about the Civil War. He told the Harvard researchers, "I am living in the present -- enjoying life and good health while it lasts."
You've Gotta Have Friends continued...
Other studies have confirmed the health-promoting power of social connections. At the UCLA School of Medicine's geriatrics division, Teresa Seeman, PhD, evaluated adults in their 70s over a seven-year period. She found that those with satisfying social relationships remained more mentally alert over the course of the study, with less age-related mental decline than people who were more isolated.
No one is certain exactly how a social network may help you stay healthy, although some research has shown that men and women who live alone tend to eat less well, which could jeopardize their physical and mental well-being. People with social connections also may have stronger disease-fighting immune systems.
"We're still struggling to understand it," says Vaillant. "People who use alcohol or are depressed are less likely to have social support, and thus personal relationships are an indicator that you're leading the rest of your life pretty well."
At RAND, a policy research "think tank" in Santa Monica, behavioral scientist Joan Tucker, PhD, says that having people in your life can make you feel loved and cared for, which can enhance your mental well-being. At the same time, a spouse or close friend can also remind you to go for walks or take your medication, which can have benefits for your physical health as well.
"Having someone prod you to get out and exercise might not make you feel loved in the short run - in fact, it may be quite irritating," says Tucker. "But it can be very effective in getting people to change their behaviors in positive ways."
Staying Mentally Active
Curiosity and creativity help transform older people into seemingly younger ones, says Vaillant, even if their joints ache and even once their days of enjoying free access to the office copying machine are a distant memory. Individuals who are always learning something new about the world, maintaining a playful spirit, and finding younger friends as they lose older ones also are making the most of the aging process.
The course of your own aging, argues Vaillant, is not written in stone, or even in your ancestry. Yes, he says, there may be genes that influence longevity, but because everyone has many good and many bad longevity genes, they tend to average out.
Even if your present lifestyle isn't what it should be, it's never too late to change. "It's a little like opening an IRA," says Vaillant. "The earlier you start one, the better, but no matter what your age, it's still worth doing." Everyone can make lifestyle changes that can move them in the direction of aging well.
Clinical St Joseph's Villa
I am doing clinical at St Joseph's Villa today. It is Sunday so I went to the LDS churchand in half an hour I am going to go to mass. I've been to lots of church services at hospitals and nursing homes and this was one of the best. I enjoyed how the residents participated. They had two Elders from a ward or branch prepare the sacrament and then they held a microphone for two of the residents who read the prayer. I thought that was very sweet and meaningful for the residents. It's one thing to go to church in a nursing home and listen and it's another to go and actively participate.
I liked the tags on the wheelchairs, "LDS, take me to church." Very nice. I wonder if the mass will say "Catholic, take me to church."
I was talking to a resident who was happy because one of our students did her makeup. I asked her if she'd done her fingernails and she said "no, I don't have any polish." I told her I'd bring some the next time I came and she asked when I was coming. I then went to the third floor and I smelled fingernail polish. It was one of our old students who is now an activity aide. She said she would go up the third floor and paint the other residents nails when she was done. SCORE!
I liked the tags on the wheelchairs, "LDS, take me to church." Very nice. I wonder if the mass will say "Catholic, take me to church."
I was talking to a resident who was happy because one of our students did her makeup. I asked her if she'd done her fingernails and she said "no, I don't have any polish." I told her I'd bring some the next time I came and she asked when I was coming. I then went to the third floor and I smelled fingernail polish. It was one of our old students who is now an activity aide. She said she would go up the third floor and paint the other residents nails when she was done. SCORE!
Friday, December 14, 2012
UNAR NEW SKILLS TO BE TESTED
Beginning and Ending Procedures
Essential Behaviors to All Skills
Skill Task Listing
The following is a listing of skill tasks that you may be asked to demonstrate. Following each task is a list of the steps that should be performed to demonstrate the task. You must be ready to correctly demonstrate each step. The bolded statements are very, very important.
CRITICAL CRITERIA
***Critical criteria include behaviors that are part of EVERY skill tested.
They include:
1. Infection control and body substance precautions (Following all rules of medical asepsis)
2. Safety (Protecting resident and self from physical harm)
3. Residents’ rights (Taking action to prevent or minimize emotional stress to resident)
4. Communication (Explaining procedure to resident prior to initiating it)
5. Recognizing and reporting changes (Observing and reporting abnormalities)
BEGINNING PROCEDURE ACTIONS
1. Wash hands thoroughly prior to entering room or when in room
· Hand washing: Demonstrating hand washing is necessary and is evaluated as part of the critical criteria.
2. Assemble needed equipment
3. Go to resident’s room, knock, and pause before entering
4. Introduce self by name and title
5. Identify the resident by facility policies and address them by name
6. Ask visitors to leave the room and inform them where they may wait
7. Provide privacy throughout procedure; pull curtains, shut door, properly cover patient as needed
8. Explain procedure to resident; speak clearly, slowly and directly to resident, maintaining face to face contact whenever possible
9. Answer resident’s questions about the procedure
10. Allow resident to assist as much as possible
11. Raise the bed to a comfortable working height
ENDING PROCEDURE ACTIONS
1. Position resident comfortably
2. Return bed to lowest position
3. Leave signal cord, telephone and water within reach
4. Perform a general safety check
5. Open curtains
6. Care for equipment following policy
7. Wash hands
8. Let visitors know they may return
9. Report completion of task & observation of any abnormalities and record actions and observations
REQUIRED
VITAL SIGNS
BLOOD PRESSURE
1. Clean ear pieces and diaphragm with antiseptic wipe
2. Position residents arm resting on firm surface with palm up
3. Wrap cuff around arm with bladder over artery 1” above antecubital space- cuff even and snug.
4. Place ear pieces in ears (directed forward towards eardrum) and place the diaphragm over artery
5. Inflate cuff to no more than 180mm/Hg or may use pulse obliteration method, candidate choice
6. Deflate cuff, note systolic reading, and note point of diastolic reading
7. Accurate reading within 4mmHg window on both systolic & diastolic
8. Accurately record blood pressure
TEMPERATURE (Tympanic, Oral or Axillary with electronic thermometer) (Examiners choice)
Tympanic:
1. Place tympanic thermometer cover on
2. Ask person to turn his head so ear is in front of you, put new probe cover on
3. Pull back on the ear (gentle, firm) to straighten the ear canal and insert probe gently into ear canal directed toward nose
4. Start the thermometer
5. Wait until you hear a beep or flashing light and remove
6. Read the temperature and record accurately
Oral/Axillary-
1. Ask the person if they have eaten or consumed a beverage, cold or hot or smoked within the last 15 minutes.
2. Place a sheath on the probe
3. Correct placement for obtaining oral reading or axillary reading
4. If necessary, hold the probe in place for oral
5. Leave the probe in place until the instrument beeps
6. Remove the probe sheath from the probe and dispose of properly
7. Replace the probe
8. Read the temperature and record accurately
RADIAL or APICAL PULSE
1. Locate pulse at the correct site
2. Count pulse for 30 sec. and double or count for 1 full min. accuracy within + or – 4 beats per minute
3. Document accurately
RESPIRATORY RATE
1. Count respirations for 30 sec. and double or count for 1 full min. Accuracy within + or - 2 breaths
2. Document Accurately
REQUIRED
HANDWASHING
1. Don’t touch the sink with your uniform
2. Turn water to warm
3. Wet and soap hands
4. Wash hands with fingers down for 15-30 seconds, including wrist, nails and between fingers
5. Rinse with fingertips down
6. Use dry paper towel to dry hands
7. Use a paper towel to turn off faucets
8. Immediately discard paper towels in trash without touching to your other hand
****You will be asked to complete 5 of the following:
SKILL 1
PRESSURE ULCER PREVENTION
1. Demonstrate 2 ways to prevent pressure ulcers:
For example:
a. Proper use of bed cradle
b. Elbow/heel protector
c. Using pillows to reduce skin to skin contact
d. Making sure sheets are wrinkle free
2. Explain 2 other ways to prevent pressure ulcers
For example:
a. Changing position frequently
b. Good nutrition and hydration
c. Provide good perineal care (keep resident clean and dry)
d. Be careful of the resident’s skin (no shearing or friction)
e. Check resident’s skin carefully-provide good skin care
f. Assist your resident to the bathroom frequently
g. Encourage mobility
h. Use pressure reducing devices
SKILL 2
POSITION FOLEY CATHETER/BAG/TUBING
1. Secure tubing to resident’s inner thigh or abdomen
2. Place tubing over leg
3. Position tubing to facilitate gravitational flow, no kinks
4. Attach to bed frame (not over or on side rail) always-below level of bladder
5. Keep catheter bag from touching floor
SKILL 3
OXYGEN
1. Demonstrate correct placement of O2 nasal cannula (place prongs following the contour of the nasal passage, tubing around ears and under chin (not behind head)
2. When asked by nurse-demonstrate how to check the oxygen flow meter and verbalize actions needed if flow rate is not accurate. Do not adjust the flow of oxygen-if incorrect, alert the nurse immediately
3. Verbalize 3 oxygen use guidelines
For Example:
a. Avoid lighting matches or smoking around oxygen use
b. Ensure that all electrical equipment is in good repair
c. No kinks in the tubing
d. Make sure the device is placed correctly on the resident
e. Do not remove the mask or nasal cannula, unless you are specifically told to do so by a nurse
f. Make sure the water level in the humidity bottle does not get too low
g. Provide oral care frequently
h. Watch for signs of skin irritation behind the person’s ears, over his or her cheeks, or around his or her ears and nose
i. Check to make sure oxygen is flowing
SKILL 4
OCCUPIED DRAW SHEET CHANGE
1. Place clean draw sheet on clean surface within reach (chair, over-the-bed table)
2. Provide privacy throughout procedure
3. Lower head of bed, placing resident in supine position
4. After raising side rail, assist resident to turn onto side, moving toward raised side rail
5. Loosen draw sheet, roll soiled draw sheet toward resident
6. Place and tuck in clean draw sheet on working side (this must be done before turning resident)
7. Raise side rail and assist resident to turn onto clean draw sheet
8. Remove soiled linens/draw sheet, avoiding contact with clothes, and place in appropriate location within room –never on floor
9. Pull and tuck in clean draw sheet, finishing with sheet free of wrinkle
SKILL 5
APPLY COLD COMPRESS
1. Cover cold compress with towel or other protective cover (compress should not be placed on bare skin without covering)
2. Properly place on correct site as directed by skills examiner
3. When asked by examiner, verbalize frequency of checks and how long you would leave compress on resident (initially check after 5 minutes/do not leave on resident for more than 20 minutes)
4. Assess for redness, swelling, irritation and or pain if this occurs remove compress and report to nurse immediately
SKILL 6
MEASURE AND RECORD FLUID INTAKE
1. Calculate intake in mL
2. Measure on a flat, level surface
3. Record intake accurately within +/- 25 mL's of nurses reading
SKILL 7
CONVERTING OUNCES TO ML’S- 30 mL’s = 1 ounce
1. Convert ounces to mL
2. Record amount accurately within +/- 25 mL's of nurses reading
SKILL 8
MEASURE/RECORD URINE OUTPUT
1. Place container on flat surface, measure accurately in mLs
2. Dispose of properly into toilet
3. Rinse and dry container
4. Remove gloves, wash hands
5. Record output accurately within +/- 25 mL's of nurses reading
SKILL 9
CONSCIOUS CHOKING
1. Candidate is able to identify symptoms of choking, asks resident “Are you choking?”
2. Call for help
3. Stands behind resident and wraps arms around resident’s waist
4. Places the thumb side of the fist against the resident’s abdomen
5. Positions fist slightly above navel
6. Grasp fist with other hand, press fist and hand into the resident’s abdomen with an inward, upward thrust
7. Candidate should indicate that they would repeat this procedure until it is successful or until the victim loses consciousness
SKILL 10
OBTAIN AND RECORD WEIGHT AND HEIGHT
WEIGHT
(Standing scale only)
1. Move weights to zero before assisting resident on to scale
2. Assist resident to stand on scale
3. Ensure resident is balanced and centered on the scale with arms at side
4. Accurately record weight within +/- 0.25 lbs. of nurse's measurement
HEIGHT
STANDING
1. Assist resident to stand on scales
2. Resident is balanced and centered on the scale with arms at side
3. Raise folded measuring bar above residents head, open and lower gently until bar rests on top of the head (not hair)
4. Accurately record height within +/- 0.5 inch of nurse's measurement
SKILL 11
APPLICATION OF ANTI-EMBOLISM STOCKINGS (TED hose)
1. Explain what position resident should be in when applying stocking- apply while resident is in bed or with feet elevated
2. Hold foot and heel of stocking and gather up stocking – turning the stocking inside out down to the heel, aids in application
3. Smooth up and over leg so hose is even, snug and not twisted or wrinkled
4. Heel and toe in proper location
5. The toe hole may be on the top or bottom of the toes, depending on the manufactures design
SKILL 12
PASSIVE RANGE OF MOTION 2 JOINTS -Examiners choice
1. Exercise passively 2 joints
2. When asked by examiner, explain or demonstrate that you understand to never exercise past the point of pain or resistance
3. Provide support for joint
4. Avoid fast jerky movements; demonstrate flexion, extension, adduction, abduction and rotation if applicable
5. Repeat exercise at least 3 times or as ordered
SKILL 13
MOVING AND POSITIONING RESIDENTS -Examiners choice
With each of the above positions you must demonstrate:
· Raise side rail while turning patient except on side you are working on
· Demonstrate proper body mechanics
· Maintain residents proper alignment at all time, for all positions
1. Draw Sheet:
· Move using a draw sheet (2 persons): Provide support for resident’s head. Grasp rolled draw sheet near residents shoulder’s and hips
2. Fowlers:
· Position in Fowler’s (high Fowler’s is 60 -90 degrees; semi-Fowler’s is 30-45 degrees; knees may be elevated approximately 15 degrees
3. Supine:
· Position in supine, in proper anatomical alignment
4. Chair/Wheelchair:
· Position in chair or W/C: provide good alignment-upper body and head erect, back and buttocks against back of chair, feet flat on floor or on W/C footrests
5. Sims (Semi Prone):
· Position in Sims /Semi prone on the correct side as directed by examiner,
Left: Resident left side lying, right leg flexed, lower arm behind resident.
Right: Resident right side lying, left leg flexed, lower arm behind resident.
Provide good alignment. Place a pillow under the head, upper arm and flexed leg
6. Lateral: (Right or Left)
· Position lateral/side-lying on the correct side as directed by examiner. Provide good alignment. Place a pillow between legs, behind back and under arm
· Note: For enema position place resident in left Sims or left lateral position
SKILL 14
ASSISTING TO AMBULATE
Demonstrating proper use of gait belt
1. Resident should have footwear with non-skid soles
2. Sit resident up, allow to dangle
3. Apply gait belt properly around resident's waist; avoid restricting circulation or breathing, or injury to skin
4. Assist resident to stand while holding gait belt. Grasp the gait belt at each side, not the front. Do not allow resident to hold onto you around your neck while transferring
5. Maintain own body mechanics while assisting resident to stand
6. Walk at resident’s side or slightly behind (on weak side, if resident has a weak side)
7. Demonstrate proper use of assistive devices (walker, cane-should be place on resident’s strong side)
SKILL 15
PIVOT TRANSFER FROM A BED TO A WHEELCHAIR/ Demonstrating proper use of gait belt
1. Lock the bed wheels
2. Resident should have footwear with non-skid soles
3. Position wheelchair close to bed on residents’ strong side
4. Move or remove foot rests from wheelchair
5. Lock wheelchair brakes
6. Lower bed and rails
7. Sit resident up, allow to dangle
8. Apply gait belt properly around resident's waist; avoid restricting circulation or breathing, or injury to skin
9. Assist resident to stand while holding gait belt. Grasp the gait belt at each side, not the front. Do not allow resident to hold onto you around your neck while transferring
10. Maintain own body mechanics while assisting resident to stand
11. Transfer to the strong side by pivoting on the strong side toward the wheelchair, using proper technique
12. Position resident properly in wheelchair with residents hips against back of seat
13. Remove gait belt without harming resident
14. Place foot rests under residents’ feet
SKILL 16
FEEDING THE DEPENDENT RESIDENT
1. Check that the name and diet on the meal tray matches the name of resident receiving it
2. Positions the resident in an upright position. Minimum 60 degrees
3. Wash and dry resident's hands before feeding
4. If resident wears dentures check to make sure dentures are in
5. Protects clothing from soiling by using napkin, clothing protector, or towel
6. Describes the foods being offered to the resident and maintain eye level contact while feeding resident
7. Offer fluid frequently
8. When asked by examiner, explain the pace and amount when feeding resident (offer food in small amounts, allow resident to chew and swallow)
9. Wipe resident's hands and face during meal as needed
10. When asked by examiner verbalize need to stop feeding when complications occur and report to nurse
For Example:
a. Choking
b. Persistent coughing
c. Mouth sores
d. Drooling
e. Cyanosis
f. Difficulty swallowing
11. Leave resident clean and in a position of comfort
SKILL 17
DENTURE CARE
1. Before handling dentures, protect dentures from possible damage (line the bottom of the sink with a towel/ washcloth or fill with water)
2. When asked by examiner, explain that water for cleaning dentures should be lukewarm (not hot or cold)
4. Brush dentures under running water with brush and paste provided
5. Place dentures in denture cup with water, adding cleaning tablet (if available), and cover with lid and allow to soak
6. Perform mouth care while dentures are out of the mouth
SKILL 18
LOG ROLLING RESIDENT WITH HIP FRACTURE PRECAUTIONS
1. Use at least 2 persons
2. Lower head of bed as flat as possible
3. Do not roll resident onto injured side
4. Place abduction splint or pillows between legs to support hip
5. On the count of “three” roll person in a single movement, being sure to keep the person’s head, spine and legs aligned
SKILL 19
ORAL CARE FOR AN UNCONSCIOUS RESIDENT/ASPIRATION PRECAUTIONS
1. Verbalize frequency of oral care (every 2 hours)
2. Place towel or drape under the resident’s head
3. Position resident (as resident’s medical condition indicates) to prevent aspiration:
a. Position resident in supine position with head to side or side lying (lateral) to prevent
aspiration or with HOB elevated and head turned to side, as resident’s medical condition
indicates
4. Insert swab/sponge tip gently into resident’s mouth
5. Do not use toothpaste/toothbrush unless approved by nurse
6. Rotate against all tooth surfaces, mucous membranes and tongue
7. Clean resident’s lips
8. Moisturize lips
9. Report abnormalities such as bleeding gums
SKILL 20
BACK RUB/MASSAGE
1. Place resident in a sitting or lateral position
2. Pour small amount of lotion into palm of hand and rub hands together to warm lotion
3. Apply with gentle pressure, using both hands from buttocks to back of neck without pulling skin, using long firm strokes
4. Use short circular strokes across the shoulders using both hands
5. Perform backrub for 3-5 min. or as ordered
6. Asses skin condition
7. Remove excess lotion
8. When asked by examiner, verbalize actions needed if redness or skin break down are noticed. Do not rub reddened area and report immediately to nurse
SKILL 21
FOOT/TOENAIL CARE
1. Inspect for cracked, broken nails/skin and between toes
2. Do not clip toenails
3. Soak feet in warm water
4. Dry feet completely including between toes
5. Apply lotion if desired but not between toes
6. Apply socks/shoes
7. Report abnormalities
SKILL 22
DRESSING/UNDRESSING RESIDENT (Must dress and undress)
1. Demonstrate how to properly dress/undress resident with hemiplegia
2. Provide privacy during entire procedure
3. Dress weak side first
4. Undress weak side last
SKILL 23
SHAVING WITH RAZOR BLADE
1. Place towel to protect resident’s clothing
2. Soften beard with warm washcloth and apply shaving cream
3. Gently pull skin taut
4. Use short strokes of razor in the direction the hair is growing
5. Rinse razor often
6. Rinse and dry resident’s face
7. Apply after shave if desired
8. Dispose blade in sharps container
SKILL 24
PROVIDE PERI-CARE (male or female examiners choice)
FEMALE
1. Assist resident in removing clothing, only as necessary, exposing only area being washed. Provide privacy (remembering dignity)
2. Obtain bath basin with water of a safe and comfortable temperature
3. Apply appropriate cleanser preferred by resident to wash cloth
4. Separate the labia, clean inside the labia downward from front to back (clean to dirty). Then wash the outside of the labia from front to back starting outside the labia and then going to the inside of the thighs. Repeat until the area is clean, using a different part of the wash cloth for each stroke
5. Rinse and gently dry each area thoroughly after washing
6. Turn the resident on their side
7. Clean the anal area from front to back
8. Rinse and gently dry each area thoroughly after washing
9. Redress resident
MALE
1. Assist resident in removing clothing, only as necessary, exposing only area being washed. Provide privacy (remembering dignity)
2. Obtain bath basin with water of a safe and comfortable temperature
3. Apply appropriate cleanser preferred by resident to wash cloth. Cleanse the penis from tip to base (clean to dirty). Repeat until the area is clean, using a different part of the wash cloth for each stroke
a. If male is uncircumcised retract the foreskin by gently pushing the skin toward the base of the penis and clean as directed above. Replace foreskin after drying thoroughly
4. Rinse and gently dry each area thoroughly after washing
5. Turn the resident on their side
6. Clean the anal area from front to back
7. Rinse and gently dry each area thoroughly after washing
8. Redress resident
SKILL 25
ASSISTING WITH A BEDPAN/FRACTURE PAN
1. Positions the bedpan/fracture pan under the resident correctly (If using a fracture pan, the flat side should be toward the back of the resident)
2. Raises head of bed to a comfortable level
3. Place tissue within reach of resident
4. Position call light within reach of the resident
5. Provide privacy
6. Gently removes bedpan
7. Provide or assist with peri-care as needed
8. Empty bedpan in toilet
9. Rinse, dry and store bedpan in proper location
10. Washes/assists resident to wash and dry hands
11. Record results accurately
SKILL 26
COLLECTING A STOOL SPECIMEN
1. Properly fill out label given and place on specimen container
2. Using a tongue depressor take a sample of feces from the bedpan or specimen collection device
3. Note color, amount and quality of the feces
4. Dispose of tongue depressor in a disposable bag
5. Empty remaining contents of bedpan or specimen collection device into toilet
6. Put lid tightly on the specimen cup
7. Place specimen cup into transport bag
8. Wash hands
9. Take the specimen cup to the designated location
Subscribe to:
Posts (Atom)