Bonnie Freeman, RN, MSN, ANP
Journal of Hospice and Palliative Nursing. 2013;15(3):147-153.
Abstract and Introduction
Abstract
Providing symptom-based care during the last days or hours of life in a hospital setting requires a complex set of skills and interactions. Often, nurses are unaware of medications they can request and nursing orders they can write within their scope of practice. This deficit in knowledge can often result in unnecessary patient and family suffering. The CARES tool, developed by this author as part of a doctor of nursing practice research project through Azusa Pacific University for the City of Hope National Medical Center, a 300-bed cancer research center in southern California, is an acronym organized educational tool that addresses the priority needs of comfort, airway, restlessness and delirium, emotional and spiritual support, and self-care. Prompts are provided for nurses on common symptom management needs of the dying based on 29 references cited in this article and the National Consensus Project for Palliative Care Clinical Practice Guidelines. The CARES acronym format was designed to help nurses stay focused and provide a method to inventory necessary tasks to address during the often chaotic and stressful last few days to hours of a patient's life.
Introduction
The CARES tool is a pocket-size, card reference that provides acronym organized prompts to address the most common symptom management needs of the dying identified in literature as c omfort, a irway management, restlessness and delirium, e motional and spiritual support, and s elf-care.[1–5] Prompts are provided for the nurse to consider regarding orders to obtain or nursing actions to implement for symptom management, possible resources for support, communication opportunities, suggestions on education needs for the dying patient and his/her family, and recommendations for methods to address compassion fatigue and professional grieving for the health care provider. Nurse's independent actions remain governed by individual comfort levels and by state and country scope of practice. The CARES tool does not provide specific drug dosages because of the wide variety of provider preference, and it is intended to be nurse driven. Many of the suggestions can be initiated at any time during the course of caring for a terminally ill patient and his/her family.
The CARES tool was designed to complement and build upon previous education obtained from professional organizations such as the Hospice and Palliative Care Nurse Association, certification examinations, and the End of Life Nursing Education Consortium programs. It is intended to be a bridge between current evidence-based knowledge and application of the knowledge to bedside nursing care.
The intentional use of an acronym format was utilized to encourage parallels to be drawn to other treatment acronym-based formats such as American Heart Association's ACLS (Advanced Cardiac Life Support) and BCLS (Basic Cardiac Life Support) in an effort to elevate the importance and respect for the unique skills required to effectively care for the dying and their family. Care of the dying may not require the same technical skills, but the communication and associated supportive skills qualify care of the dying an acute event.[6–8]
The CARES tool debuted as a poster presentation at the 19th International Congress on Palliative Care in Montreal, Quebec, Canada, in October 2012, and received a 98% (n = 125) positive approval rating from expert palliative care providers when asked to formally evaluate the tool. Reviewers felt the CARES tool (a) could assist in the education of health care staff, (b) could be easily implemented, and (c) effectively prompts the obtaining of orders and supportive measures for the dying patient and his/her family.
Suggested Symptom Management
Sixty percent of all deaths occur in hospitals, and 80% to 90% of the deaths will be expected.[1,3,6,9–12] Many hospitals do not have guidelines specific to the care of the dying. If a protocol or pathway is available, it is often initiated too late or not at all because of the unwillingness of the ordering provider to make the diagnosis of dying necessary to implement the protocol.[3,10] This current system results in 50% of terminally ill patients dying in pain and 80% experiencing suboptimally treated dyspnea and terminal delirium before death.[13] These dismal statistics can be attributed to the discomfort ordering clinicians have for the use of opioids, barbiturates, antipsychotics, and sedatives during the dying process.[1,4,7,9,12–14]
Knowledge deficits, misconceptions, and unfounded beliefs continue to result in barriers affecting pain and symptom management for the dying.[4] The fear of causing harm is counterproductive for dying patients and often results in undertreatment and further suffering.[2,13,15] Literature confirms there is no limit to opioid sedation. It can be titrated to whatever dosage is required to relieve a patient's pain and maintain desired respiratory status.[2,3,5] The use of opiates and sedatives to manage dyspnea at end of life remains complicated by knowledge deficits and personal attitudes, often resulting in the denial of dignified comfort measures for the dying.[2,4,16] Concepts of intent and double effect can greatly assist in guiding humane and ethical symptom management concerns but are often poorly understood.[7,9] The intent or desired outcome of pain and symptom management is to relieve suffering not to provideeuthanasia.[9,14,17]
Double effect can be defined as a decision to utilize an intervention with potential adverse effects or harm when it is determined that the benefits outweigh the risks, and the health care provider's intent is to relieve the patient's suffering.[15] If an actively dying patient writhing in pain is given a bolus of morphine and dies a few moments later, his/her death can be attributed as much to the disease process as the opioid.[6,7] The double effect was the benefit of reliving a patient's pain. It outweighed the risk of causing the patient to die a few moments sooner. Relieving pain and eliminating suffering are the intent and should be the focus of end-of-life (EOL) care.[6]
Nurses remain the primary decision makers for titration and obtaining necessary medications and orders to provide compassionate care for patients. Their role as a patient advocate can ensure that all components to provide a peaceful death are in place to support a dying patient and family in their final journey. Education and experience in care of the dying are essential, and the use of resources such as the CARES tool can assist in this process.
Components of Cares Tool
C: Comfort
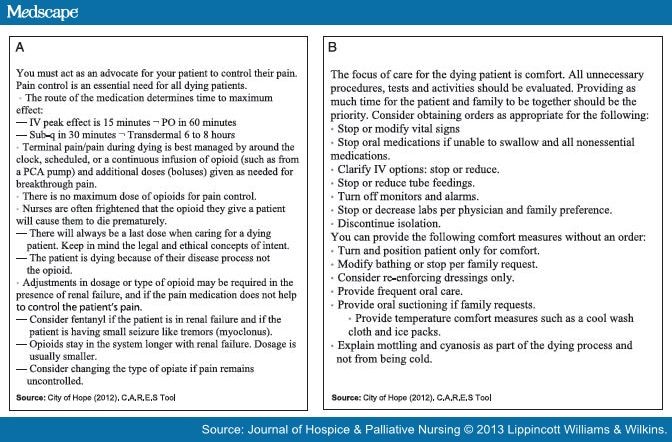
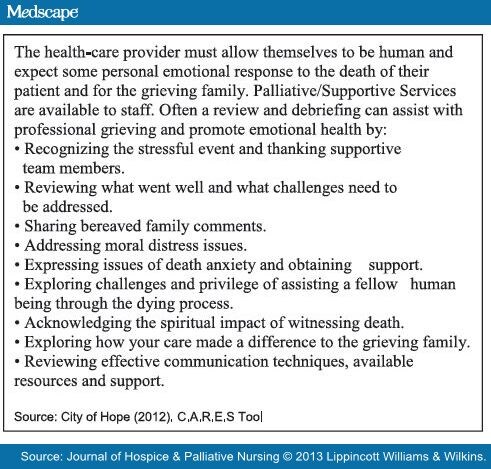
The CARES tool addresses the broad subject of comfort. Pain management (Figure 1A) is a primary focus. Specific opioids and dosing are avoided in the CARES tool because of the variety of agents available and unique preferences of providers. A baseline knowledge and understanding of opioids and pain management are essential for the effective use of the CARES tool. A 1-page section in the CARES tool on the vast topic of chronic pain management could never fully address all issues. Key points provided are intended to prompt important considerations regarding route of administration, decisions to provide continuous basal dosing, titration, renal failure, ineffective opioids, and adjustments for small seizure-like activity (myoclonus).[2,5] The important concepts of intent and double effect are listed as a reminder of the barriers to providing effective EOL pain management.
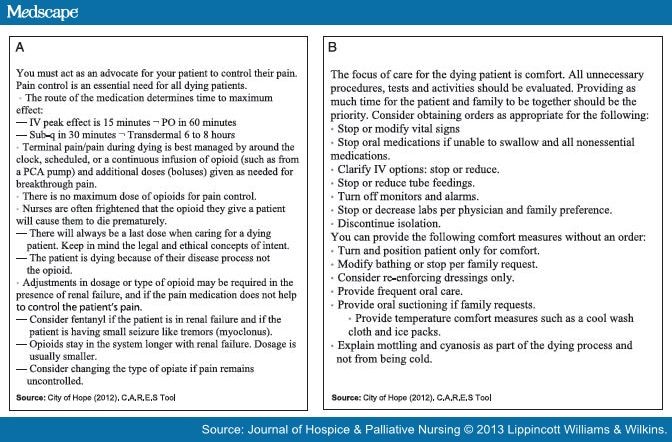
Figure 1.
A, CARES pain management. B, General comfort. Abreviations: PO, per os; IV, intravenous; PCA, patient-controlled analgesia.
The comfort section (Figure 1B) also addresses unnecessary procedures, tests, and activities not essential to maintaining the physical comfort of the dying patient. Nurses should evaluate routine tasks such as the obtaining of vital signs, use of monitors and alarms, and blood draws. A primary question one should ask is what will be done with this information? If no further treatment is planned, the task could be eliminated.[1,2,18] An emphasis must be placed on providing the patient and family maximum time together for closure so procedures such as bathing, turning, and dressing changes may need to be modified or eliminated. It is important to communicate with the patient and the family in this decision process as the elimination of some procedures could be interpreted as providing lesser or inadequate care.[1,6,18]
An understanding of the physiological changes that occur during the dying process is necessary for the effective use of the CARES tool. Procedures to control temperature extremes, edema, and cyanosis are ineffective during the dying process but can provide comfort to the family as they perceive basic care is still being provided.[1,6,12] Supplying a cool washcloth for a family member to place on the forehead of their dying loved one will not alter the patient's rising body temperature, but it conveys to the family the respect the nurse holds for the patient and confirms that care is still continuing. This is an example of the importance of a nurse's humanity and an example of how the family needs to be a focus of nursing care[1,18] (Figure 1B).
The comfort section of the CARES tool addresses the concern that everything possible was done to make the patient and family comfortable.
A: Airway
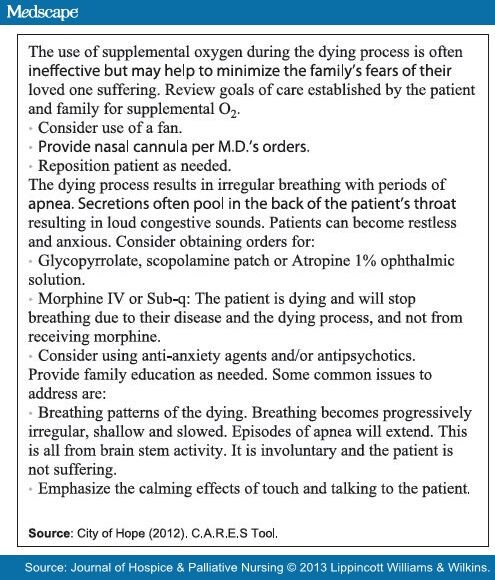
The airway section in the CARES tool explores the management of dyspnea (Figure 2). A basic understanding of the physiologic changes occurring during the dying process is essential and will greatly influence the effectiveness of teaching provided to the patient and family members.
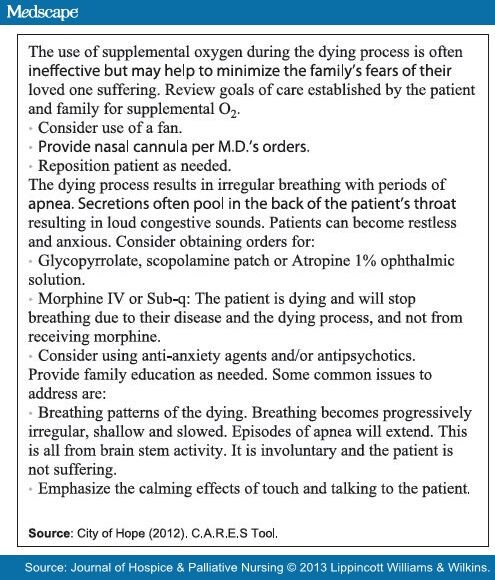
Figure 2.
CARES airway. Abreviations: IV, intravenous; MD, medical doctor; Sub-q, subcutaneous.
The use of opiates and sedatives to manage dyspnea at end of life is again re-enforced. As stated previously, knowledge deficits and personal attitudes can contribute to further suffering and need to be addressed through further education and experience.[2,4,16]
Morphine remains the criterion standard for prevention of the sensation of suffocating commonly present in the terminally ill.[7,15] Its use often seems counterproductive, but research has found if a dying patient can be kept calm, and his/her oxygen needs to be minimized, the perception of air hunger and suffocation can be reduced.[2,6,10] Suffocation can be one of the most frightening and devastating symptoms the dying must endure.[6,7] The use of antipsychotics and/or antianxiety agents may be necessary to further reduce oxygen requirements. A calm and supportive environment and use of therapeutic touch by the family and nurse are essential.[1,2,18]
The loss of the ability to swallow and control airway secretions is common in the dying process. The primary agents used to address the increase in pooling oral-pharyngeal secretions are glycopyrrolate (Robinul), scopolamine patch, or atropine 1% ophthalmic solution given bucally.[2,3,19] Specific drug and dosages vary with institution and provider preference and were intentionally omitted in the CARES tool. Any of the 3 agents help to control increased oral-pharyngeal secretions associated with the "death rattle."[5,18] This accumulation of secretions does not appear to cause additional suffering for the patient as it occurs within the last few days to hours before death, but it can be extremely disturbing to the family.[1,2,6,18] Oral suctioning is typically ineffective as secretions rapidly reaccumulate. Oral suctioning will increase patient restlessness, further deprive the patient of oxygen, and take precious time away from patient and family grieving and closure.[6,16]
An important education point when addressing airway issues recommended in the CARES tool is the explanation and reassurance families require regarding the irregular, gasping, and agonal-appearing respirations that can occur in the unconscious dying patient hours to moments before death. Families need to know this irregular breathing is involuntary and common in the dying process, and it is not an indicator of suffering.[1,12,18] Again, an understanding of the physiological changes occurring within the body as brain stem function becomes the sole source of respiratory stimulus is essential to enhance the teaching and reassurance so desperately needed by the dying patient's family (Figure 2).
When considering the airway section of the CARES tool, the nurse should ask themselves what can be done to help the patient breathe easier and what else can be said to reassure the family that their loved one is not suffering.
R: Restlessness and Delirium
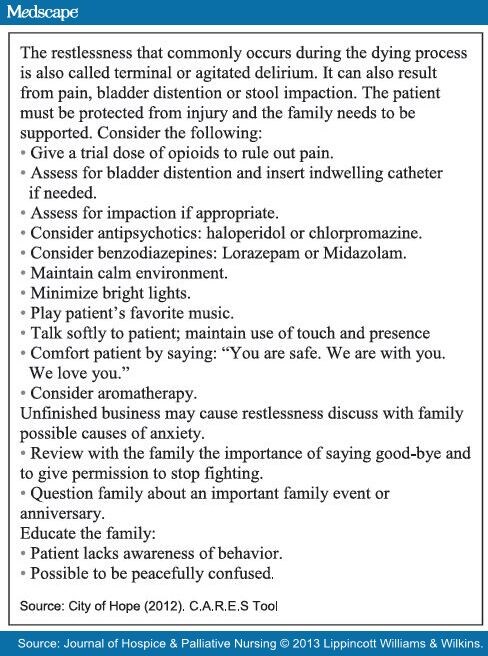
Terminal or restless delirium occurs in 25% to 85% of actively dying patients.[20] The symptoms include restlessness, agitation, confusion, nightmares, and hallucinations. Uncontrolled pain, particularly in the elderly, can cause confusion and florid delirium. Effective pain management can actually maintain mental clarity.[6] Lorazepam, midazolam, chlorpromazine, and haloperidol are the most frequently used medications for the management of terminal and restless delirium.[9,15,20,21] Providing familiar music, sounds, smells, and a calm nonstimulating atmosphere and the use of touch and verbal reassurance can greatly assist in the reduction of restlessness.
The family may require assistance to explore possible causes of a patient's restlessness such as unresolved conflicts, the desire to see a specific loved one again, or concern over abandoning their family. The nurse should encourage the family to reassure the patient and assist where possible to resolve any "unfinished business."[1,18]
Some forms of delirium can be resistant to standard medical management and require more aggressive sedation to control dangerous thrashing or combative behavior. This can be frustrating for family as the need for increased sedation will limit final communication and closure.[20,21] Families are frightened and confused as terminal delirium can present as a dramatic change in personality and behavior. Effective teaching on the common occurrence of terminal delirium as part of the dying process and reassurance from health care providers is needed.[2,6]
The restlessness section of the CARES tool should prompt nurses to review all possible causes of the patient's restlessness or delirium and to ensure any additional reassurances, support measures, and education are provided (Figure 3).
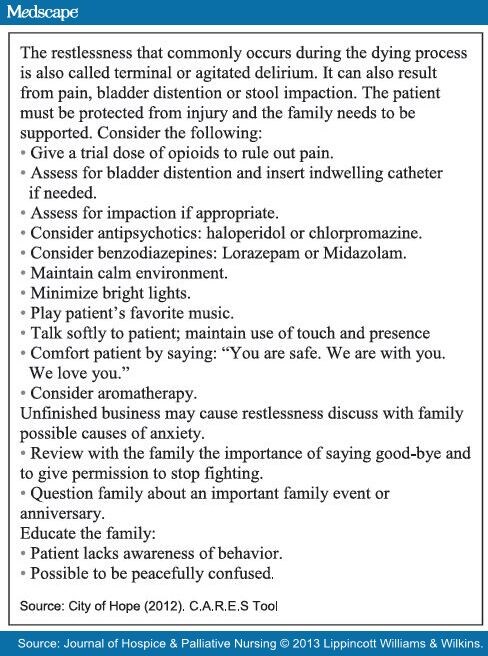
Figure 3.
CARES restlessness and delirium restlessness.
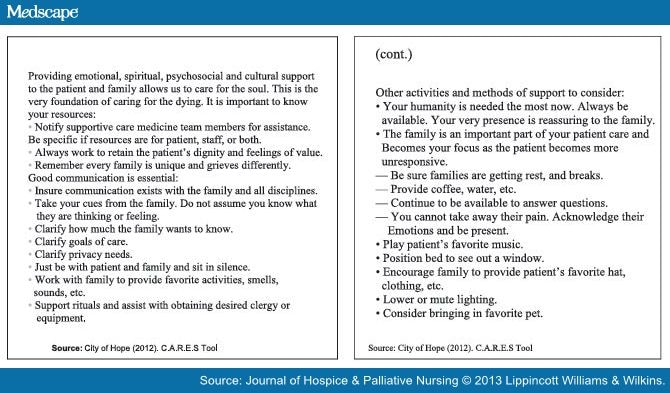
E: Emotional and Spiritual Support
The CARES tool includes the well-documented need for emotional and spiritual support.[1,2,13,18,20–22] Addressing fears of the dying process, abandonment, the unknown, identifying signs and symptoms of nearing death versus suffering, helping families understand emotional withdrawal by the dying patient, and the continued need for touch are common teaching points.[1,2,18] The slowing of physical and mental processes typically seen in the dying can create increased emotional, psychological, and spiritual distress for the patient and family.[1,2,20]
Supportive efforts should focus on assisting both patient and family members.[2,6,23] Long-term psychosocial and mental health issues can develop as a result of prolonged, unrelieved stress associated with the perceived suffering of a loved one.[6,10,20,24] Positive perceptions of the dying processes can influence family coping abilities, grief and bereavement, and future ability to adjust to loss.[20] There is a continual need for emotional and physical support, re-enforcement of decision process, and acknowledgement of grief.[8,25] Clear and open communication is essential. Issues of perceived suffering should be addressed and readdressed to help comfort the family and assist coping.[6,20,23] Nurses need to recognize and embrace the power of their humanity and value it as strongly as any technical skill.[26] The very presence of a health care provider willing to take the time to listen and share in the emotional and spiritual journey of the dying process signifies respect and acknowledges the value of the patient and his/her family.[1,26,27]
When reviewing the emotional and spiritual needs of the patient and family, consider what else can be done to promote a comfortable and peaceful death, and what additional measures may be required to support the family (Figures 4A and Figures 4B).
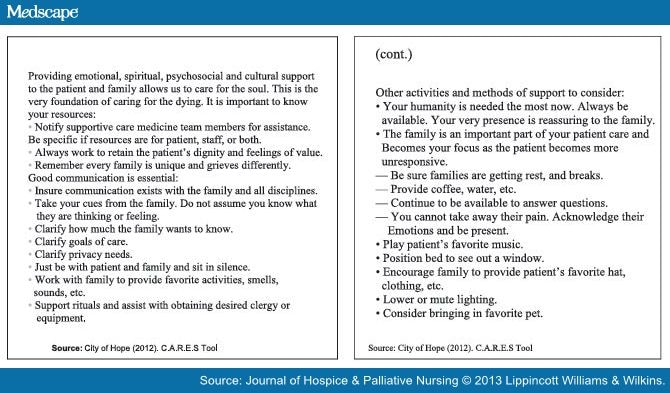
Figure 4.
CARES emotional support.
S: Self-care
The final section of the CARES tool is self-care. Caring for the dying and their families can be very stressful for the health care provider.[11,23] Moral distress can develop as personal core values and perceptions of futility remain unaddressed.[14] Moral distress and compassion fatigue become magnified as health care staff struggle in the role of patient advocate.[6,8] Psychological distress, compassion fatigue, vicarious stress, and secondary traumatic stress syndrome are just some of the terms used to define the resultant loss of self-worth, anxiety, depression, helplessness, dread, anguish, and compromised integrity that can develop when caring for the traumatized, critically ill, and dying.[23,25] Prior knowledge of the importance of self-care is required to fully understand and embrace this important concept contained in the CARES tool.
The CARES tool is designed to remind the nurse to debrief and seek professional and peer support as needed. It is essential for a nurse to accept the normal human need to grieve and to recognize the emotional, spiritual, and psychological damage that can occur when grieving is suppressed.[24,28]
When considering the self-care section of the CARES tool, the nurse should evaluate his/her own emotional status and how it is impacted by providing care to the dying. The CARES tool encourages debriefing, communication, and seeking methods to promote emotional health (Figure 5).
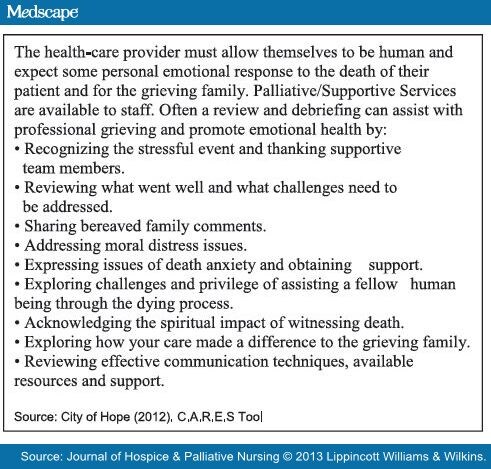
Figure 5.
CARES self-care.
Case Study
Mr F. was a 78-year-old gentleman with a history of cardiomyopathy and acute renal insufficiency. He presented to the emergency room complaining of generalized 8/10 chest pain and acute fatigue. He was short of breath, emaciated, pale, and diaphoretic with a blood pressure of 82/40 mm Hg. An echocardiogram showed an ejection fraction of less than 5%. Mr F. knew he was dying and requested do-not-resuscitate status. He was placed on a morphine patient-controlled analgesia at 1 mg/h and PRN boluses of 0.5 mg every 15 minutes PRN, and given oxygen per nasal cannula at 2 L/min. He was admitted to the medical unit with orders for comfort measures only. Hospice was to evaluate him in the morning.
Using the CARES tool as a guide, the nurse clarified what comfort measures meant to Mr F., obtained needed orders, and planned the following nursing actions:
Comfort: Based on the comfort section of the CARES tool, the nurse obtained orders to (a) stop all laboratory draws as no follow-up treatments would be provided; (b) change obtaining vital signs to every shift given there were no plans to treat deficits and to minimize interrupting rest; (c) reduce intravenous lines to KVO, limiting the risk of fluid overload and pulmonary edema; and (d) titrate the morphine patient-controlled analgesia to control pain and to optimize coronary perfusion and reduce the workload of the heart.
Airway: Following the CARES tool section, the nurse was aware the use of morphine is a recommended standard for the treatment of shortness of breath and planned to continue to titrate as needed. She positioned Mr F. in a comfortable upright position to promote ease of respirations and obtained an order for glycopyrrolate subcutaneous for any increased oral-pharyngeal secretions Mr F. may develop as he progresses deeper into the dying process. Mr F. found the oxygen cannula irritating and requested its removal. The nurse was aware through the CARES tool that oxygen supplementation is often ineffective in the dying process. Oxygen is considered a medication, and Mr F. had the right to refuse it.
Restlessness and delirium: Mr F. became very restless but denied chest pain. The nurse reviewed the CARES tool section on restlessness and noted the suggestion to rule out treatable causes of restlessness such as pain and bladder distention. Mr F.'s bladder was firm and distended. An order was obtained for a urinary catheter. Mr F. had an immediate output of 500 mL and began to rest more comfortably. The nurse acted on additional prompts from the CARES tool and obtained an order for haloperidol PRN in preparation of possible future restlessness and/or terminal delirium and lowered the lights in the room to maintain a calm and supportive environment.
Emotional and spiritual support: The CARES tool recommends the creation of a supportive and loving atmosphere through the presence of friends and family. Mr F. denied having any family and requested a friend be called and allowed to remain at the bedside. The nurse noted the friend was visibly upset upon arrival and took the time to explain Mr F.'s condition and to listen to the friend's concerns that Mr F. not suffer. The CARES tool emphasizes the importance of treating both the patient and family as a single unit, so the nurse listened attentively and provided education and reassurance. Mr F. appeared peaceful with the friend at the bedside. The nurse was aware of the CARES tool recommendation to help the patient and family avoid any sense of abandonment. His status was assessed frequently, and assurances were made that the nurse would be available if needed. The nurse was aware Mr F. was awake after the friend had fallen asleep. Based on the CARES tool, the nurse knew the importance of presence for emotional and spiritual comfort. The nurse sat by the bedside and held Mr F.'s hand providing reassurance and promoting additional patient comfort. Mr F. died peacefully a few hours later. The friend was supported by pastoral care and assisted with funeral arrangements. Based on prompts from the CARES tool, the nurse knew to obtain additional support from the palliative care team as needed.
Self-care: The nurse became tearful when recalling Mr F.'s death while attempting to give report to the on-coming shift. Following CARES tool recommendations, the nurse sought out support from peers. A debriefing session was provided by the manager and attended by coworkers. The nurse was encouraged to verbalize feelings and felt listened to and supported. A CARES tool suggestion to take pride in knowing the last few hours of Mr F.'s life were comfortable and peaceful was explored and provided additional emotional comfort for the nurse.
The case study is a very basic, uncomplicated example of the use of the CARES tool. It provides an example of how death can be a calm and supportive experience if the nurse is prepared and knows what orders to clarify and/or obtain, what supportive nursing measures to make, and what support systems are available.
Key Implications for Palliative Nursing
The CARES tool addresses the most common symptom management needs of a dying patient.[1,2,15,20,29] Research has helped to identify the needs of the dying, the grieving family, and the professional staff. The use of an acronym organized, generic protocol for the care of the dying such as the CARES tool incorporates this research into a readily accessible resource. It can be implemented at any point during EOL care without a formal diagnosis of dying by the ordering provider. This eliminates one of the greatest barriers to the timely and effective use of many pathways and protocols.[9,10] The CARES tool was designed to assist the nurse in the role of patient advocate with prompts on possible orders to obtain, discussions to initiate for improving communication with the patient and family, and teaching points to consider reducing family perceptions of suffering.
Future Research
The CARES tool will be part of a research project at the City of Hope National Medical Center, a 300-bed cancer research center in Duarte, California, to explore methods to improve the delivery of evidence-based care for the dying in a hospital-based setting. Additional research would be welcomed to explore the CARES tool usefulness and adaptation to home-care and long-term-care settings.
The CARES tool is the property of the City of Hope with copyright status pending. The CARES tool is available for downloading free of charge at the City of Hope Pain and Palliative Care Resource Center Web site:
http://prc.coh.org.
References
American Association of Colleges of Nursing (AACN). End of Life Nursing Education Consortium (ELNEC) program. www.aacn.nche.edu/elnec. Accessed January 2012.
American Medical Association (AMA). The EPEC project (Education in Palliative and End of Life Care). http://www.epec.net/epec_core.php. Accessed October 2012.
Costantini M, Ottonelli S, Canavacci L, Pellegrini F, Beccaro M. The effectiveness of the Liverpool care pathway in improving end of life care for dying cancer patients in hospital: a cluster randomized trial. BioMed Central Health Serv Res [open access online article]. 2010;11(13):1–10.
Walling A, Brown-Saltzman K, Barry T, Quan RJ, Wenger NS. Assessment of implementation of an order protocol for end-oflife symptom management. J Palliat Med. 2008;11(6):857–865.
Wu P. Patty Wu's Palliative Medicine Pocket Companion. San Diego, CA: Institute of Palliative Medicine; 2009.
Byock I. The Best Care Possible. New York: Penguin Group (USA) Inc; 2012.
Quill TE. AMidwife Through the Dying Process: Stories of Healingand Hard Choices at the End of Life. Baltimore, MD: The John Hopkins University Press; 1996.
Catlin A, Carter B. State of the art: reaction of a neonatal end-of-life palliative care protocol. J Perinatol. 2002;22(3):184–195.
Walling A, Asch SM, Lorenz KA, et al. The quality of care provided to hospitalized patients at the end of life. Arch Intern Med. 2010;170(12):1–13.
Ellershaw J. Care of The Dying: A Pathway to Excellence. 2nd ed. New York: Oxford University Press; 2011.
Frommelt K. Attitudes toward care of the terminally ill: an educational intervention. Am J Hosp Palliat Care. 2003;20(1):13–22.
Thurston AJ, Wilson, DM, Hewitt JA. Current end of life care needs and care practices in acute care hospitals. Nurs Res Pract. 2011;2011:1–8.
Byock I, Twohig JS, Merriman M, Collins K. Promoting excellence in end-of-life care: a report on innovative models of palliative care. J PalliatMed. 2006;9(1):137–151.
Ong W, Yee CM, Lee A. Ethical dilemmas in the care of cancer patients near the end of life. Singapore Med J. 2012;53(1):11–14.
Radha Krishna LK, Poulose VJ, Goh C. The use of midazolam and haloperidol in cancer patients at the end of life. Singapore Med J. 2012;53(1):62–66.
Del Fabbro E, Dalal S, Bruera E. Symptom control in palliative care. J Palliat Med. 2006;9(2):422–437.
Morgan J. How to improve services for dying patients in critical care: adapting protocols. Nurs Times. 2010;106(4):16–18.
Ferrell BR, Coyle N, eds. Oxford Textbook of Palliative Nursing. 3rd ed. New York: Oxford University Press; 2010.
Kamal AH, Maguire JM, Weeler JL, Currow DC, Abernethy AP. Dyspnea review for the palliative care professional: treatment goals and therapeutic options. J PalliatMed. 2012;15(1):106–114.
Brajtman S. Helping the family through the experience of terminal restlessness. J Hosp Palliat Nurs. 2005;7(2):73–81.
De Graeff A, Dean M. Palliative sedation therapy in the last weeks of life: a literature review and recommendations for standards. J Palliat Med. 2007;10(1):67–85.
Douglas C, Murtagh FE, Chambers EJ, Howse M, Ellershaw J. Symptom management for the adult patient dying with advanced chronic kidney disease: a review of the literature and development of evidence-based guidelines by a United Kingdom expert consensus group. Palliat Med. 2009;23(2):103–110.
Parish K, Glaetzer K, Grbich C, Hammond L, Hagarty M, McHugh A. Dying for attention: palliative care in the acute setting. Aust JAdv Nurs. 2006;24(2):1–25.
Sinclair S. Impact of death and dying on the personal lives and practices of palliative and hospice care professionals. Can MedAssoc J. 2011;183(2):180–187.
Peterson J, Johnson M, Halvorsen B, et al. What is so stressful about caring for a dying patient? A qualitative study of nurses' experiences. Int J Palliat Nurs. 2010;16(4):181–167.
Puchalski CM, Ferrell, BR. Making Health Care Whole:Integrating Spiritually Into Practice [electronic edition]. West Conshohocken, PA: Templeton Press; 2010.
Nichols T. Death and Afterlife: A Theological Introduction. Grand Rapids, MI: Brazos Press; 2010.
Todaro-Franceschi V. Compassion Fatigue and Burnout inNursing: Enhancing Professional Quality of Life. New York: Springer Publishing; 2013.
Keene PR, Thompson C. Educational implications of nurses' assessment and management of pain. J Hosp Palliat Nurs. 2008;10(6):370–375.